by Boston University School of Medicine
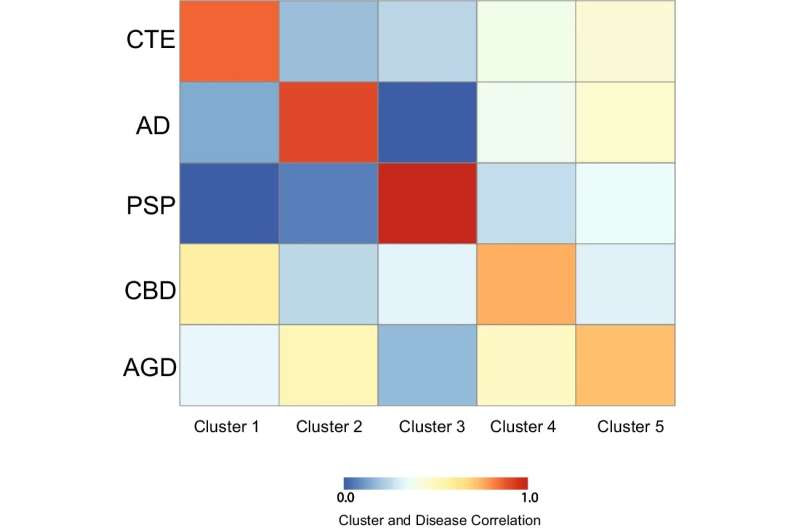
Partial Least Square regression identifies clusters of proteins that correlate with each tauopathy. Using the partial least square regression analysis, five clusters of ELISA proteins were identified and compared against each tauopathy to determine degree of correlation. Each comparison was a contrast of a single tauopathy against all other neuropathologies. Blue represents low correlation and red represents high correlation. Comparisons are adjusted for age at death and gender. Cluster 1 was most correlated with CTE, Cluster 2 with AD, Cluster 3 with PSP, Cluster 4 with CBD, and Cluster 5 with AGD. Credit: Journal of Neuroinflammation (2022). DOI: 10.1186/s12974-022-02640-6
Researchers from the BU CTE Center have found that immune-related proteins could help differentiate between neurodegenerative diseases and provide additional candidates for biomarkers or new therapeutic targets.
One of the largest challenges in neuroscience is identifying and treating neurodegenerative diseases during life, as many are only able to be diagnosed after death.
Additionally, several diseases can sometimes have overlapping clinical symptoms that makes diagnosis even more challenging, including Alzheimer’s disease (AD), Chronic Traumatic Encephalopathy (CTE), progressive supranuclear palsy (PSP), corticobasal degeneration (CBD) and argyrophilic grain disease (AGD), which highlights the critical need for better ways to identify and distinguish during life.
“We identified the protein CCL21 was specific of CTE, FLT3L was selective of AD, and IL-13 was highest in PSP. This is novel since it provides more possible biomarkers to help better identify diseases like CTE, AD, PSP, CBD or AGD during life. Additionally, it helps us better understand the mechanisms behind each disease,” says corresponding author Jonathan Cherry, Ph.D., a research health scientist at the VA Boston Healthcare System and assistant professor of pathology and laboratory medicine at Boston University Chobanian & Avedisian School of Medicine.
The researchers examined postmortem brain tissue from 127 individuals with CTE, AD, PSP, CBD or AGD. They analyzed the concentration of 71 different immune related proteins and used a statistical technique to identify if specific clusters of proteins were most correlated with a specific disease.
After determining a cluster of proteins for each disease, they took the top five proteins for each cluster to determine which protein was the strongest possible biomarker candidate. They then validated the initial results by comparing postmortem cerebrospinal fluid from individuals with CTE and AD.
“We demonstrated that the protein CCL21 was able to distinguish CTE from AD in spinal fluid, further highlighting future use as a novel biomarker for in-life diagnoses. However, an important caveat is that it’s likely there won’t be a single ‘magic protein’ for any disease diagnosis. Ultimately, these proteins will be needed to be coupled with several other biomarkers, imaging studies, and clinical symptoms to really be effective. However, here we provided more targets that can help increase the overall specificity of diagnosis,” he adds.
According to the researchers, these results highlight how important the immune system is to neurodegenerative diseases. Additionally, they suggest that better understanding of the neuroinflammatory signature that is specific to individual neurodegenerative diseases may lead to identifying more specific biomarkers for all diseases and ultimately discover novel therapeutic compounds.
These finding appear online in the Journal of Neuroinflammation.

Leave a Reply