by University of Oxford
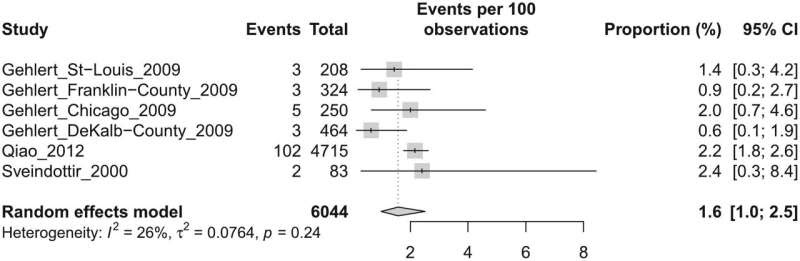
Forest plot of studies from community-based samples with confirmed diagnosis of PMDD. Credit: Journal of Affective Disorders (2024). DOI: 10.1016/j.jad.2024.01.066
About 1.6% of women and girls have symptomatic Premenstrual Dysphoric Disorder (PMDD), according to a new review of global studies published in the Journal of Affective Disorders titled “The prevalence of premenstrual dysphoric disorder: Systematic review and meta-analysis.”
Researchers led by Dr. Thomas Reilly at the University of Oxford’s Department of Psychiatry looked at studies from across the world to work out how many women and girls met the strict diagnostic criteria for the condition. The data suggested around 1.6% did—equivalent to around 31 million women and girls globally.
A higher proportion—3.2%—had provisional diagnoses, where the condition is suspected but symptoms had not been measured for a sustained period of time to meet criteria for confirmed diagnosis.
Symptoms of PMDD include mood changes (such as depression and anxiety), physical symptoms (such as breast tenderness, and joint pain), and cognitive problems (difficulty concentrating or memory complaints).
Dr. Reilly, who is a Medical Research Council (MRC) Clinical Research Training Fellow in the Department of Psychiatry at Oxford University and Specialist Registrar at the National Female Hormone Clinic, Maudsley Hospital, says the proportion of those affected could be higher than 1.6%.
“Because diagnostic criteria is so strict, this is likely an underestimation of the lifetime prevalence of PMDD, and many more women and girls may be undiagnosed. Even so, the data emphasizes that at a given timepoint there is still a significant minority of women with symptomatic PMDD, which is strongly associated with suicidal thoughts,” he said.
“There is little training around PMDD for psychiatrists or indeed medical students. Patients often find themselves falling through gaps in clinical services, such as between gynecology and mental health services. GPs’ knowledge about PMDD is also very variable. In psychiatry, we rarely consider whether a patient’s symptoms might relate to hormonal changes.
“We need better awareness and training among health professionals about this debilitating but highly treatable condition so that patients can benefit from effective, evidence-based management and support,” Dr. Reilly added.
Researchers used data from 50,659 female participants in 44 studies across six continents. They say the data challenges many preconceptions about the illness, including that it is a medicalization of “normal” menstrual symptoms, or that it was a “Western culture-bound syndrome.”
Clare Knox, an organizational psychologist who co-authored the paper and has experienced PMDD herself, said, “In a world where the health and well-being of every individual matters, the revelation that approximately 31 million females worldwide may be silently grappling with Premenstrual Dysphoric Disorder, a condition that deeply impacts their daily lives, cannot be overlooked.
“This staggering figure is a wake-up call, underscoring the urgent need for enhanced diagnostic processes, effective treatment plans, and robust support systems for those affected. More than ever, it is vital that we invest in comprehensive research and public health strategies to address and manage PMDD, ensuring that these millions of women do not face their struggles in the shadows, but rather with the full support and understanding of a society that values their health as a priority.”
More information: Thomas J. Reilly et al, The prevalence of premenstrual dysphoric disorder: Systematic review and meta-analysis, Journal of Affective Disorders (2024). DOI: 10.1016/j.jad.2024.01.066
Journal information: Journal of Affective Disorders
Provided by University of Oxford

Leave a Reply