JUNE 25, 2024
by Westmead Institute for Medical Research
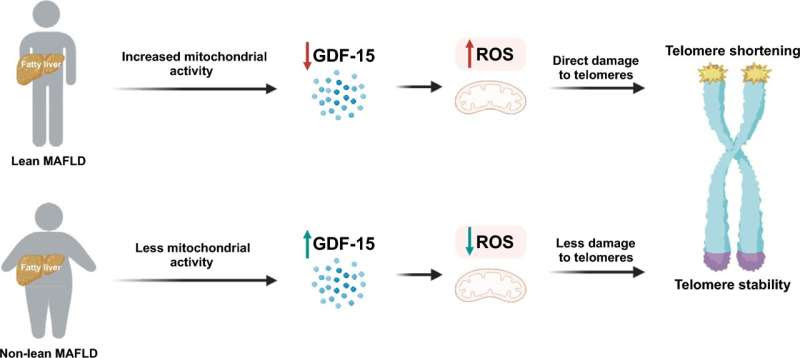
Proposed model for the differential mortality outcomes between patients
who are lean and non-lean with MAFLD. Credit: Hepatology International (2024). DOI: 10.1007/s12072-024-10701-6
A world-first research discovery from the Storr Liver Center at The Westmead Institute for Medical Research (WIMR) has identified why lean people with metabolic dysfunction-associated fatty liver disease (MAFLD) have higher mortality than their non-lean counterparts.
The research, published in Hepatology International, provides a new drug target for the development of potentially lifesaving treatments, as well as the potential to increase early detection.
MAFLD affects up to one third of the global population and is the leading cause of end-stage liver disease, liver cancer and liver transplantation. In Australia, the prevalence of MAFLD has been reported to be 20%–30% and is the most common liver disease.
Although typically associated with excess weight, obesity and type 2 diabetes, up to 20% of individuals with MAFLD are considered to be lean.
Sydney University Ph.D. student Mohammad Alarabi, first author of the study, says, “Despite being healthier overall than their overweight or obese counterparts, lean people with MAFLD have a worse long-term prognosis. We set out to understand the mechanisms that cause this seemingly contradictory outcome.”
The research team focused their efforts on telomeres—protective structures found on the end of chromosomes. Alarabi says, “Telomeres protect the end of a chromosome from becoming frayed and tangled.
“Each time a cell divides, some of the telomeres get cut off. Eventually, the telomeres become so short that the cell dies.”
The shortening of telomeres is associated with increased morbidity and mortality in several diseases.
Alarabi explains, “We hypothesized that telomere loss increases in times of substantially higher energy demands or metabolic stress. Long-term, this could lead to increased cell death and poorer outcomes.”
In this study, the research team demonstrated that growth/differentiation factor-15 (GDF-15), a protein that helps to regulate a cell’s response to injury, is reduced in lean individuals with MAFLD.
As the cells try to adapt to this reduction in GDF-15, it results in an increase in molecules known as endogenous reactive oxygen species (ROS). An increase in ROS can cause damage to telomeres and may result in cell death.
“It is the combination of a decrease in GDF-15 and increase in ROS that leads to a more rapid loss of telomeres,” says Alarabi.
“We have been able to demonstrate that the shortening of telomeres can, in part, explain the increased mortality of lean individuals with MAFLD.
“We say ‘in part’ because there is another factor that we believe has an impact on mortality rates.
“As the name suggests, ‘fatty liver’ is usually associated with excess weight and obesity. Many health professionals do not consider that a lean person potentially has a fatty liver. This means that many lean individuals are diagnosed with MAFLD much later than their non-lean counterparts, which results in delayed treatment.
“This could also partially explain the increased mortality of lean individuals with MAFLD,” Alarabi says.
The next step for the research team is to look for treatments that could stop the increase in ROS, reducing telomere loss and increasing survival rates for lean people with MAFLD.
Alarabi adds, “We also hope to develop a biomarker that could identify increased ROS, and improve early detection of MAFLD in lean individuals.”
More information: Mohammad Alarabi et al, Telomere length and mortality in lean MAFLD: the other face of metabolic adaptation, Hepatology International (2024). DOI: 10.1007/s12072-024-10701-6

Leave a Reply