by Delthia Ricks , Medical Xpress
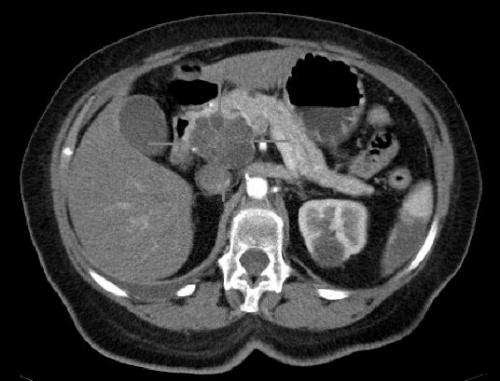
Axial CT image with i.v. contrast. Macrocystic adenocarcinoma of the pancreatic head. Credit: public domain
Medical investigators are theorizing that a combination of two treatments that activate myeloid cells may effectively treat a recalcitrant form of pancreatic cancer that thwarts conventional immunotherapy.
Mobilizing the immune system to destroy cancers has been one of the breakthrough treatments of the past decade, spurring the defeat of cancers via immunotherapies that marshal T cells to wage war against malignancies. The problem facing oncologists and their patients is that T cell-based immunotherapy works well for some cancers, but not all forms of the disease.
Activated T cells are extraordinary killers in immunotherapies, and while these lymphoid cells are effective when mobilized against some cancers, there apparently is a role for new strategies, scientists now say.
A team of cancer biologists, studying an approach that activates myeloid cells against tumors, say they are seeing positive results in the treatment of a resistant form of pancreatic cancer.
New research at the University of Pennsylvania is investigating the potential of a different type of immunotherapy in an experimental approach that relies on two immunotherapies that target myeloid cells.
Investigations of this strategy are underway in animal-model studies and early human clinical trials. The basic concept guiding both the animal model and human research hinges on a deceptively simple concept: Combining two treatments that activate myeloid cells may prove successful against tumors where more conventional T cell-based immunotherapies have failed.
Writing in Science Immunology, cancer biologists at UPenn’s Perelman School of Medicine found that the combined targeting of the myeloid cell-activating receptors CD40 and dectin-1 can unleash potent antitumor immunity.
“By co-targeting myeloid activation molecules, we leveraged the myeloid compartment as a therapeutic vulnerability,” wrote Dr. Max M. Wattenberg, lead author of the newly-published, mouse-model research.
“Myeloid cells in solid tumors expressed activation receptors including the pattern recognition receptor dectin-1 and the TNF receptor superfamily member CD40. In mouse models of checkpoint inhibitor-resistant pancreatic cancer, co-activation of dectin-1, via systemic β-glucan therapy, and CD40, with agonist antibody treatment, eradicated established tumors,” added Wattenberg, who conducts research in the division of hematology and oncology at Perelman School of Medicine.
Launching a dual-pronged approach underscores myeloid cells’ potential as potent cancer fighters, especially against a particularly resistant tumor type that failed to respond to the single therapy approach.
In the analyses, Wattenberg and a team of collaborators used systemic β-glucan in tandem with CD40 agonist antibody therapy and found that this combination successfully activated anti-tumor T cell responses, where conventional T cell-targeted immunotherapy had not.
Myeloid cells are immune cells that mature in the bone marrow and play an important role in anti-tumor immune activity. There are three myeloid cell lines: granulocytic, erythroid and megakaryocytic. These cell lines include a long roster of with familiar names, such as erythrocytes; platelets; the family of granulocytes—basophils, eosinophils and neutrophils; monocytes and myeloid dendritic cells.
Perhaps more so than their lymphoid cell counterparts, myeloid cells can be reprogrammed to be immunosuppressive when they enter the tumor microenvironment, Wattenberg and colleagues report.
In their laboratory research involving animal models of human pancreatic ductal adenocarcinoma, the team found that established pancreatic tumors that were resistant to T cell–targeted immunotherapy could be eradicated with their new strategy. Targeting both myeloid cell activating receptors—CD40 and dectin-1—created a potent myeloid-based response against tumors, overcoming the naturally immunosuppressive signals of the tumor microenvironment.
“Antitumor activity was dependent on … T cells but did not require classical T cell–mediated cytotoxicity or blockade of checkpoint molecules,” Wattenberg wrote. “Rather, targeting CD40 drove T cell–mediated interferon-gamma signaling, which converged with dectin-1 activation to program distinct macrophage subsets to facilitate tumor responses.”
To be clear, the antitumor activity of dectin-1/CD40 activation required T cells but it was completely independent of T cell cytotoxicity and immune checkpoint pathways, the findings demonstrate.
Wattenberg and colleagues emphasize that antitumor activity also required interferon-gamma and intra-tumoral macrophages. The findings demonstrate that the targeting of myeloid cell activation pathways can generate strong antitumor immune responses against tumors that are resistant to conventional immunotherapy.
“These findings define a previously-undescribed immunotherapy paradigm via co-activation of complementary myeloid signaling pathways,” concluded Wattenberg, noting that a clinical trial studying a combination immunotherapy treatment for patients with pancreatic ductal adenocarcinoma is underway.
More information: Max M. Wattenberg et al, Cancer immunotherapy via synergistic coactivation of myeloid receptors CD40 and Dectin-1, Science Immunology (2023). DOI: 10.1126/sciimmunol.adj5097
Journal information: Science Immunology
© 2023 Science X Network

Leave a Reply