JULY 11, 2024
by Brian Burns, Massachusetts General Hospital
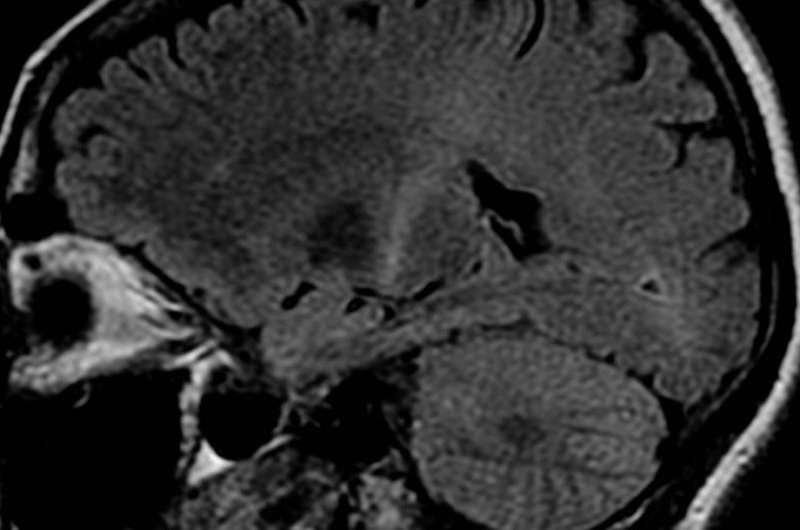
An MRI with increased signal in the posterior part of the internal
capsule which can be tracked to the motor cortex consistent with the diagnosis of ALS. Credit: Frank Gaillard/Wikipedia
Immune system dysregulation and elevated inflammation contribute to the development of the fatal neurodegenerative condition amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease.
In research published in The FASEB Journal, repeated infusions of certain immune cells delayed ALS onset and extended survival in mice, and also reduced markers of inflammation in an individual with the disease. The work was conducted by investigators at Massachusetts General Hospital.
“This makes the first step towards a Phase I clinical trial of our new cell therapy for ALS, which is now in the planning stage,” said senior author Mark C. Poznansky, MD, Ph.D., Director of the Vaccine and Immunotherapy Center, an attending physician in General and Transplant Infectious Diseases Medicine at Massachusetts General Hospital, and a professor of Medicine at Harvard Medical School.
Previous work by the group of Ruxandra F. Sîrbulescu, Ph.D., assistant professor of Neurology and co-corresponding author of the article, showed that direct application of purified B cells, which are immune cells known to produce antibodies, can reduce inflammation and promote recovery in mice with skin or brain injuries.
The benefits resulted from a process termed pligodraxis, in which the B cells adopt immunoregulatory and neuroprotective characteristics to support the repair of damaged tissues in an injured environment.
“What we observed early on in preclinical studies has been a remarkable effect of B cells in the context of brain lesions—both brain structure and function were protected by treatment with these cells, which made us consider applying them as a therapeutic in the context of neurodegenerative disease,” Sîrbulescu said.
In this latest research, the team assessed the effects of B cell infusions in mice prone to ALS and in a person living with the disease.
In mice, repeated intravenous treatments of B cells from donor mice significantly delayed disease onset, extended survival, reduced cell death, and decreased a marker of neurodegeneration.
In the human patient, repeated infusions of donor B cells were safe and led to decreased levels of multiple inflammatory markers.
“We were able to show that B cells, which can be readily obtained from the blood, could treat ALS in a well-established mouse model of the disease, and we obtained permission from the US Food and Drug Administration and our hospital to try this treatment approach in an individual with ALS,” said Poznansky.
“We were able to show safety and efficacy, as well as how the B cell therapy worked in mice, and we demonstrated that our approach was safe and feasible in a human. This is a first study of its kind to apply B cells to the treatment of ALS and sets us up for a trial of this new treatment approach to a currently incurable disease.”
More information: Ruxandra F. Sîrbulescu et al, Allogeneic B cell immunomodulatory therapy in amyotrophic lateral sclerosis, The FASEB Journal (2024). DOI: 10.1096/fj.202302659R
Journal information: FASEB Journal

Leave a Reply