by Julia Rinner, Technical University Munich
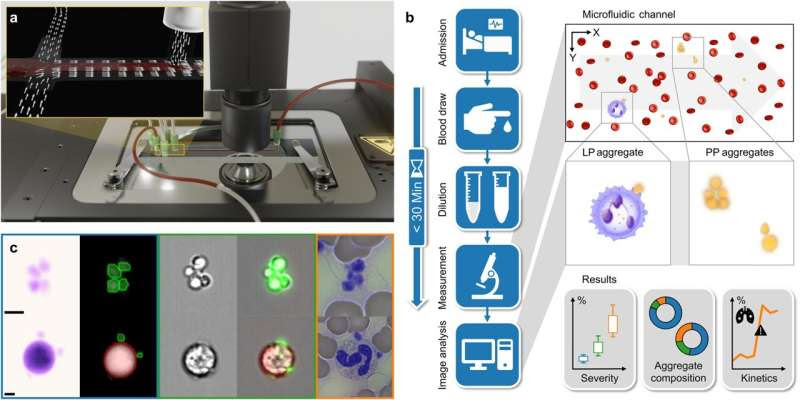
Novel image-based flow cytometry enables the identification of cell aggregates and their components. a Scheme of a flow cytometry setup including a DHM and a microfluidic chip. The insert illustrates the applied principle of hydrodynamic focusing in two dimensions. b Study workflow: consisting of admission of patients to the hospital, blood draw, sample dilution, measurement in the microfluidic channel (within 30 min from collection), and image analysis. c Platelet aggregates (top row, PP) and leukocyte-platelet aggregates (bottom row, LP) were captured with different imaging techniques as reference. From left to right, exemplary images detected by DHM in false color, DHM images with single cells detected by the algorithm (blue box), brightfield images with an AMNIS imaging flow cytometer, AMNIS images of brightfield merged with the fluorescence images (green box), and images of a blood smear (orange box) are depicted. The green circles (DHM images) indicate that the algorithm detects a platelet, whereas green-fluorescent cells (AMNIS images) represent CD61-labeled cells. Likewise, red circles represent leukocytes detected by DHM, while CD45-labeled cells are red fluorescent. Credit: Communications Medicine (2023). DOI: 10.1038/s43856-023-00395-6
Researchers at the Technical University of Munich (TUM) have developed a method for assessing the number and structure of aggregated blood platelets (or thrombocytes) that can potentially help quantify the risk of a severe COVID-19 infection. As a result, they have identified a predictive biomarker for the seriousness of a COVID-19 infection.
This will allow physicians to adjust treatment at an early stage. The researchers used a method from image-based flow cytometry that permits the rapid analysis of interactions between large numbers of blood cells. The research is published in the journal Communications Medicine.
When infected with the SARS-CoV-2 virus, the human body produces a series of immune responses. One of them involves platelets, also known as thrombocytes, sticking to immune cells to form clumps, or aggregates, of cells in the bloodstream. In a study using image-based flow cytometry, a team of researchers working with Oliver Hayden, a professor of biomedical electronics, demonstrated a rapid rise in concentrations of platelet aggregates in patients admitted to intensive care with COVID-19 infections.
This enabled them to identify a biomarker for predicting the risk of severe illness in COVID-19 patients. The result was made possible by the optimal interdisciplinary conditions offered by the central TranslaTUM institute to TUM engineers for collaboration with medical researchers at Klinikum München rechts der Isar.
The analysis began with a blood sample taken from the test subjects. A few drops of blood are needed to count thousands of blood cells and their aggregates within seconds using image-based flow cytometry.
Prof. Hayden, the head of the study, says, “Another big advantage of this method is that we neither have to treat nor mark the samples. Using standardized methods, we can investigate them directly without aggregation losses caused by high shearing forces. In the future, this cost-effective method could help quantify interactions between the coagulation system and the immune system.”
The close proximity of patients to the lab when taking samples permits the blood to be tested immediately. This rules out effects from the aging of samples, which also causes aggregates to form.
The researchers investigated blood samples from 36 intensive care patients (aged 32 to 83) admitted to the hospital with a SARS-CoV-2 infection classified as moderate to severe. The results showed that the number of aggregated thrombocytes in the blood samples of severely ill patients was significantly higher than in moderately ill patients and definitely in healthy blood donors.
With regard to the cell aggregates, the researchers found that the number of aggregates and their composition changed gradually in line with the severity of the COVID-19 infection and that these changes occurred at an early stage before complications appeared. The aggregates were typically made up of fewer than 10 thrombocytes. In extreme cases, it was observed that up to two-thirds of all thrombocytes in a patient were aggregated.
A high concentration of cell aggregates was seen in all COVID-19 patients admitted to intensive care. This simple diagnostic method based on blood cell aggregates has the potential to identify high-risk patients at an early stage and improve their care.
The interdisciplinary team of engineers and medical researchers now plan to transfer what they have learned to other diseases. They believe that the method described here could also function with cardiovascular disease or cancers.
More information: Christian Klenk et al, Platelet aggregates detected using quantitative phase imaging associate with COVID-19 severity, Communications Medicine (2023). DOI: 10.1038/s43856-023-00395-6
Journal information: Communications Medicine
Provided by Technical University Munich

Leave a Reply