by Medical University of Vienna
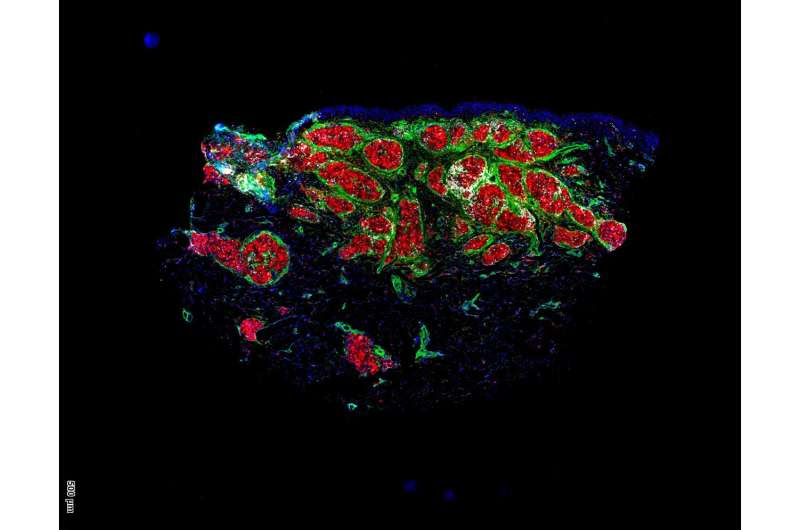
Immunofluorescence staining makes granulomas glow red with a green border (macrophages with fibroblasts). Credit: MedUni Vienna/Anna Redl
A research team led by Georg Stary (Medical University of Vienna and CeMM) has identified a new approach to treating the inflammatory disease sarcoidosis. In a clinical study, the inhibition of a specific signaling pathway showed clear success in the treatment of granulomas in the skin. This opens up new therapeutic paths for sarcoidosis and similar inflammatory diseases.
The results are published in the journal The Lancet Rheumatology.
Sarcoidosis is an inflammatory disease that is difficult to treat and affects around 15 to 20 out of every 100,000 people. In this disease, tiny clusters of inflammatory cells called granulomas form in the affected organs. These granulomas can affect normal tissue and lead to inflammation and fibrosis, which ultimately limits the functionality of affected organs.
In their study, the researchers from MedUni Vienna and CeMM (Research Center for Molecular Medicine of the Austrian Academy of Sciences) focused their attention on possible new therapeutic approaches for sarcoidosis.
They chose the mTOR (mechanistic target of rapamycin) signaling pathway, which is known to regulate metabolism and growth in many cell types, as mTOR activation was observed in granulomas of different tissues from multiple patients. Sixteen patients with granulomas of the skin and other organs were included in a clinical study at the Department of Dermatology.
The researchers used the mTOR inhibitor sirolimus, which was first approved in 1999 to prevent organ rejection after kidney transplants. It had already shown promise in preclinical models of sarcoidosis.
Complete remission of symptoms in some cases
Sirolimus was first administered topically (as a cream) and then systemically (as an oral solution) to test its effect on the skin granulomas. Topical treatment proved unsuccessful, perhaps because the granulomas—compact structures in the skin—are difficult to penetrate from the surface.
In contrast, systemic treatment was successful in 7 out of 10 patients, who completed the study, and some even experienced complete regression after four months of treatment and no recurrence up to two years later.
Interestingly, patients who responded to the systemic treatment had higher mTOR expression in their granuloma fibroblasts than those who did not.
“We suspect that, unlike broad-spectrum immunosuppressants, mTOR inhibition targets both immune and non-immune cells in granulomas, which prevents a recurrence of tissue granulomas,” says study leader Georg Stary.
Multi-center study to confirm results
The clinical study also suggests an effect of systemic treatment on granulomas in other vital organs, although it is difficult to draw concrete conclusions due to the small number of patients.
The researchers are now planning a multi-center clinical trial with more patients to confirm the skin results and further test the drug’s efficacy, especially in lung involvement, which is present in 90% of sarcoidosis sufferers.
“Given the rarity of sarcoidosis and the fact that mTOR inhibitors such as sirolimus are no longer patented, research interest from the industry is limited. This shows the importance of investigator-initiated studies and academic research,” says Georg Stary, indicating the academic character of this study.
In future work, the researchers want to investigate the significance of mTOR and other signaling pathways in other non-infectious granulomatous skin diseases such as necrobiosis lipoidica, which is often associated with diabetes. Stary hopes that their research will lead to further targeted therapies for these neglected diseases.
More information: Anna Redl et al, Efficacy and safety of mTOR inhibition in cutaneous sarcoidosis: a single-centre trial, The Lancet Rheumatology (2024). DOI: 10.1016/S2665-9913(23)00302-8
Journal information: The Lancet Rheumatology
Provided by Medical University of Vienna

Leave a Reply