by Mary Van Beusekom, Johns Hopkins University
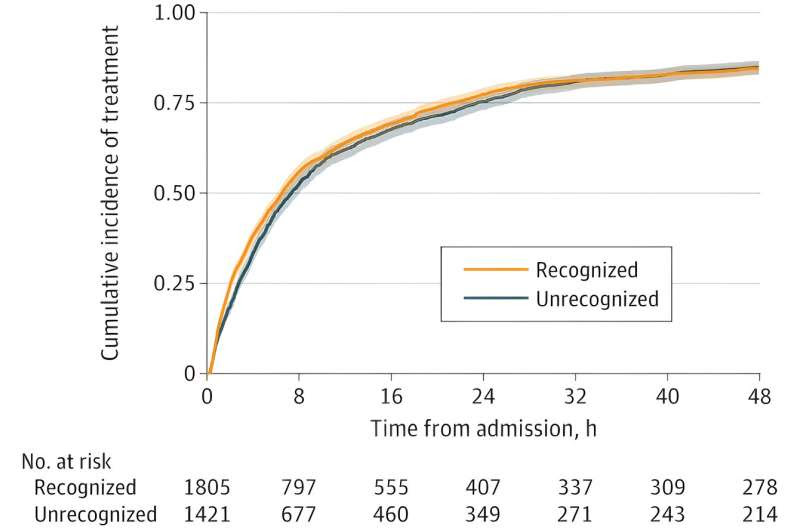
Cumulative Incidence of Treatment During the First 48 Hours of Hospitalization. Comparison of patients with COVID-19 admitted after July 1, 2020, with first arterial oxygen saturation (SaO2) measurement below 94% who had recognized or unrecognized need for COVID-19 therapy (concurrent pulse oximeter saturation [SpO2] at 94% or 94% and higher, respectively). Credit: JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.30856
A study led by Johns Hopkins University researchers suggests that the use of pulse oximeters in hospitalized COVID-19 patients often overestimated true arterial oxygen saturation (SaO2), especially in those of minority race, and led to delayed therapy in a high proportion of patients of all races.
For the study, published today in JAMA Network Open, the researchers used linear mixed-effects models to evaluate the relationship between the overestimation of oxygen saturation in COVID-19 patients using pulse oximetry and time to receipt of the drugs remdesivir or dexamethasone, hospital length of stay, risk of hospital readmission, and in-hospital death among 24,504 patients at 186 U.S. hospitals with concurrently measured pulse oximetry oxygen levels (SpO2) and SaO2 from March 2020 to October 2021.
Average patient age was 63.9 years, 41.9% were female, 41.4% were white, 32.2% were Hispanic, 16.0% were Black, and 10.4% were Asian, Native American or Alaskan Native, Hawaiian or Pacific Islander, or another race.
The investigators also assessed a subset of 8,635 patients admitted after July 1, 2020, who didn’t need immediate COVID-19 therapy based on an SpO2 reading of 94% or higher without supplemental oxygen.
“Observational data and laboratory studies suggest that pulse oximeters systematically overestimate arterial oxygen saturation among patients from minority racial and ethnic groups, leading to a greater risk of occult hypoxemia, generally defined as a true arterial oxygen saturation (SaO2) below 88% with an oxygen saturation by pulse oximetry (SpO2) in a normal range above 92%,” the study authors wrote.
Minorities had more hidden low oxygen
Pulse oximetry overestimated SaO2 for Black (adjusted mean difference, 0.93 percentage points), Hispanic (0.49 percentage points), and other race (0.53 percentage points) patients compared with white patients. In the patient subset, compared with white patients, Black patients were at significantly higher risk of having pulse oximetry measurements that masked the need for COVID-19 medication (adjusted odds ratio [aOR], 1.65).
Occult hypoxemia (hidden low oxygen) was noted in 18.3% of Black patients, 20.9% of Hispanic patients, and 19.7% of patients from other racial and ethnic minority groups (19.7%), compared with 13.0% of white patients. At the individual level, occult hypoxemia was seen in 4.9% of SpO2−SaO2 pairs (4.9%) among Black patients, 5.1% among Hispanic patients, and 4.5% among other racial minority patients, compared with 3.5% among white patients.
Of note, Black patients had the lowest rate of in-hospital death and the shortest length of hospital stay.
Patients with an unrecognized need for COVID-19 medication were 10% less likely to receive it (adjusted hazard ratio, 0.90) and had higher chances of readmission (aOR, 2.41), regardless of race. There was no link between the unrecognized need for COVID-19 therapy and in-hospital death (aOR, 0.84) or length of stay (mean difference, −1.4 days).
Pulse oximeter inaccuracy was highest among patients of minority race, suggesting that these groups would be disproportionately affected on a population level, but about 13% of patients who had occult hypoxemia and over 43% of patients with an unrecognized need for COVID-19 medication by pulse oximetry were white.
“These results suggest that although racial and ethnic disparities exist in measurement of oxygen saturation by pulse oximetry, overestimation may increase the risk of hospital readmission regardless of patient race,” the researchers wrote. “The relationship between overestimation of oxygen saturation with timing of COVID-19 medication delivery and clinical outcomes remains unknown.”
Improved pulse oximeter accuracy is critical to the delivery of timely and equitable care to COVID-19 patients. “The implications of pulse oximeter errors likely extend to other acute respiratory illnesses and oxygen supplementation in chronic respiratory disease, which necessitate ongoing investigation,” they concluded.
More information: Ashraf Fawzy et al, Clinical Outcomes Associated With Overestimation of Oxygen Saturation by Pulse Oximetry in Patients Hospitalized With COVID-19, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.30856
Journal information: JAMA Network Open
Provided by Johns Hopkins University

Leave a Reply