by European Society of Cardiology
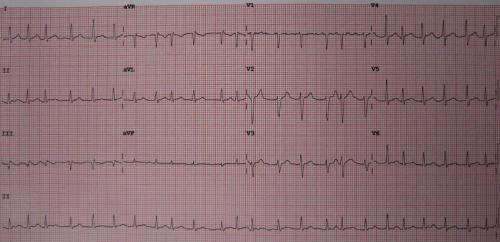
A 12 lead ECG showing atrial fibrillation at approximately 150 beats per minute. Credit: James Heilman, MD/Wikipedia/CC BY-SA 3.0
A novel software tool set to improve the management of elderly atrial fibrillation patients with multiple conditions is being designed by the EHRA-PATHS consortium. The latest updates on this clinical innovation will be presented at EHRA 2023.
Scientific coordinator Professor Hein Heidbuchel said, “EHRA-PATHS is developing a standardized approach to ensure that patients with atrial fibrillation receive evidenced-based therapies for the comorbidities that underlie or complicate their heart rhythm disorder.”
Atrial fibrillation is the most common heart rhythm disorder, affecting more than 40 million people worldwide. Patients with atrial fibrillation have an average of five co-existing conditions including high blood pressure, coronary artery disease, heart failure, obesity and chronic kidney disease. These comorbidities have a negative impact on survival. In addition, three-quarters of atrial fibrillation patients take at least five medications.
EHRA-PATHS is a multicenter international project focused on integrated care for patients with atrial fibrillation and at least one additional chronic condition. The multidisciplinary program is being coordinated by the ESC and the European Heart Rhythm Association (EHRA). An EHRA-PATHS survey of healthcare professionals previously reported that the lack of an integrated care model was hindering referrals to specialist services for atrial fibrillation comorbidities.
Results of patient interviews, presented for the first time at EHRA 2023, highlighted the need for integrated care and interprofessional working to optimize the health of patients with multimorbid atrial fibrillation. The in-depth interviews included 30 atrial fibrillation patients with two or more additional conditions from Belgium, Greece, Poland, Spain and the Netherlands. The average age was 73 years and 37% were women. The most common comorbidity was high blood pressure, followed by high cholesterol, obesity, hypothyroidism and diabetes. Interviewees stressed the need for better communication between primary care and hospitals. Some had multiple appointments at different locations and were frustrated with the unintegrated care. While respondents had some knowledge about the relationship between comorbidities and atrial fibrillation and were motivated to make adjustments, they lacked formal education on how to implement and maintain lifestyle changes.
EHRA-PATHS investigators have defined 22 comorbidities that are relevant in patients with atrial fibrillation. For each, the consortium has created concise care pathways to check for or exclude whether a given comorbidity is present, to guide its further evaluation, and to ensure its effective management. The care pathways are now being integrated in a software tool that will assist healthcare personnel to evaluate atrial fibrillation patients in a systematic and comprehensive way. “This is the cornerstone of the overall aim of the project, which is to improve outcomes of patients with atrial fibrillation by systematic detection and management of underlying conditions, and by multidisciplinary referral or collaboration where needed,” said Professor Heidbuchel.
The software will be evaluated in a clinical study involving 65 hospitals in 14 European countries. To establish a baseline picture, in part one of the study, researchers will evaluate the management (assessment and treatment) of risk factors and comorbidities in approximately 1,300 patients aged 65 years and older with newly diagnosed atrial fibrillation. Part two will be a randomized controlled trial in 1,080 patients assessing whether allocation to the software tool improves management of atrial fibrillation compared with usual care.
The trial will focus on 12 comorbidities: hypertension, hyperlipidaemia, heart failure, overweight/obesity, renal insufficiency, smoking, diabetes, coronary heart disease, valvular disease, physical activity, chronic obstructive pulmonary disease/asthma and alcohol consumption. The primary endpoint is the number of risk factors and comorbidities that are identified and for which treatment is initiated during base mapping (part one) and at the end of the randomized controlled trial (part two). Secondary endpoints include atrial fibrillation symptom burden, quality of life, patient and healthcare professional satisfaction, referrals to other disciplines and cost-effectiveness.
Professor Heidbuchel said, “Our vision is that EHRA-PATHS will demonstrate through its clinical trial that a systematic approach to comorbidities, based on a software tool with interdependent care pathways, leads to better multidisciplinary management of patients with atrial fibrillation. If the project succeeds, it will have delivered a tool to the medical community to improve atrial fibrillation management, and to make it more uniform all over Europe and beyond.”
Provided by European Society of Cardiology

Leave a Reply