COMMENTARY
These Steps Can Help Patients Keep Their Feet on the Ground
Bruce Berry, MD
DISCLOSURES | August 19, 2024
Almost every pickleball player has fallen at some time, and all players are at risk for future falls. The data are staggering. The Centers for Disease Control and Prevention (CDC) estimates that 1 in 4 adults over age 65 fall each year, resulting in 3 million visits to the emergency room; 300,000 hip fractures; and 32,000 deaths annually.
Okay, we can’t blame pickleball for all of that; most falls in pickleball do not result in serious harm. But as the sport becomes more common, particularly among older people, serious falls are increasingly likely to be a problem for players.
Indeed, I just fell playing last month. I found myself running after a ball that was hit a little too far away. My upper body got ahead of my feet, and down I went. I was lucky and only bruised my ego! Other causes of falls include running into someone or something, tripping over your own feet, landing awkwardly after a jump, or sustaining an injury to the lower extremity — a twisted ankle or pulled muscle, for example.
To help your patients prevent falls, you can’t just tell them to “try harder not to fall.” As clinicians, we know that giving “try harder” advice usually doesn’t work, no matter the condition. How often do your patients respond to “you should lose some weight” or “you should exercise more”?
Instead, try actionable items. The CDC suggests four things to reduce the risk for falling: Make your home safer; have your medications reviewed for hypotension or dizziness risk; get your eyes and feet checked; and perform exercises to improve balance. Let’s translate that advice into the pickleball world.
Many of our patients are on medications that can lower blood pressure and predispose them to dizziness and falling. Because most of these medications cannot be stopped, I suggest to my patients to consider spacing their medications out over the course of the day, rather than taking everything at the same time, and ideally not shortly before playing. This practice usually is safe, particularly for once-daily medications designed to last for long periods, but you will have to decide on a case-by-case basis what is best for your patients.
Balance is heavily dependent on three body systems: vision, proprioception, and inner ear function. If your patients need corrective lenses for anything besides reading, advise them to wear their prescription glasses (or contacts) while playing. Even better would be for them to purchase a pair of prescription safety glasses, designed for sports. Not only will they see better and be more stable on their feet, but they’ll also reduce the risk for an eye injury. Also, stress the importance of regular eye exams for cataracts and glaucoma, both of which can reduce vision and negatively affect balance.
Proprioception naturally erodes with age, but additional losses can occur with diabetes, chemotherapy, and neuropathic disorders. Be extra vigilant with your patients who have these conditions, realizing that they are at increased risk for falling. Advise them to undergo a formal evaluation from a physical therapist for balance and gait safety.
Of course, many patients will not go to physical therapy, so you can recommend a few simple exercises for them to do at home to improve their balance.
Sit to stand is an easy exercise to start with. It builds core strength, which is essential for balance. Patients should sit in a firm chair, then stand up, without using the arms for assistance, then sit back down. The exercise should be repeated 20 times in a session, starting with one set daily and advancing to several sets as tolerated. I have suggested to patients to do these while watching commercials run on TV, or for a minute or two between answering emails, or even after they finish a meal when they are about to get up from the table.
Slightly more difficult, but still doable, advise and demonstrate to patients how to practice standing on one leg. This exercise is best done with something nearby to hold onto in the event that they lose their balance. The kitchen is a good place, as the counter or a chair are within easy reach. Patients should start by standing on one leg for 5 seconds, then switch to the other leg for 5 seconds. I demonstrate this to patients while in the exam room with them. As they develop proficiency, I suggest that they advance the one-leg time to 20 seconds. This exercise should be repeated for 3 minutes daily.
Another easily demonstrated exercise is walking heel to toe, as if you are walking a tightrope. Again, keep something nearby to grab in case you lose your balance. You can suggest that they work up to 10 steps, and as with any of these exercises, shorten the duration or stop if it is too hard or if it is painful.
An advanced exercise that combines the elements of stationary balance with dynamic balance is a march with exaggerated leg lifts (Figure 1). Patients should walk forward, slowly lifting the left thigh until it is almost parallel to the ground, hold that position for a few seconds, then step forward with the left leg. Repeat on the alternate side. As proficiency develops, increase both the duration of time for holding the leg up and the number of steps taken.
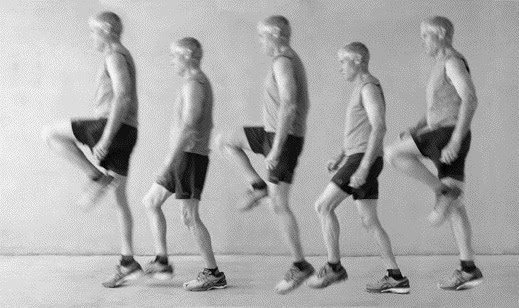
Figure 1. Slow march to improve balance.
I can demonstrate the sit to stand, stand on one leg, heel-to-toe walk, and march to a patient in the office in 2 minutes. You might consider offering your patients these fall-reducing exercises too.
The CDC reports that most hip fractures occur as a result of a fall to the side, a direction in which we do not routinely move. To build strength and improve stability in the lateral direction, your patients can practice a lateral lunge (Figure 2).
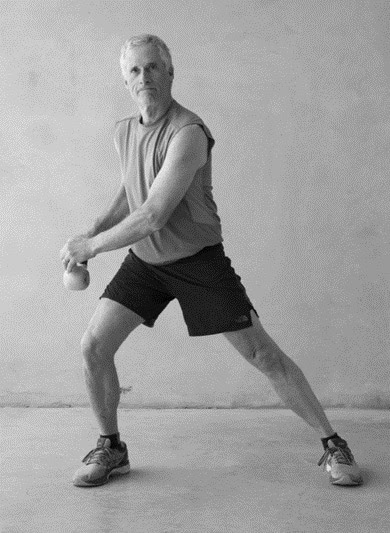
Figure 2. Right lateral lunge with optional weight.
To demonstrate this activity, start with the feet at shoulder width, standing straight up. Take a step to the right and bend the right knee while lowering the hips, hold it for a few seconds, then return to the starting position and repeat this movement on the other side. The addition of a light weight can increase the difficulty of the exercise and work the upper body, too. Starting with five lunges in each direction is an activity most players can do but will find just a little bit difficult.
Now, I know you are thinking, All great advice, but it is work and most people won’t do it. So, here is an easy one: Wear pickleball shoes! Yes, shoes designed for pickleball are different from other athletic shoes. Typical running shoes are designed for movement and support in the forward direction, but pickleball shoes are also designed for lateral movement. They are less likely to stick when shuffling laterally and offer support to prevent rolling of the foot, which can lead to foot fractures. Buying safety is easy.
Even with the best intentions, accidents happen. But with a little planning, we can help our patients minimize the risk for falling. Advise them to play within their limits, do not overextend, stay hydrated, wear glasses, communicate with their partners during the game, use the correct equipment, and practice these exercises daily.
Bruce Berry, MD, is a primary care physician in Wisconsin and a pickleball enthusiast. He is the author, with his son Andrew Berry, DO, of A Doctor’s Guide to Treatment and Prevention of Pickleball Injuries(2023).

Leave a Reply