by American College of Rheumatology
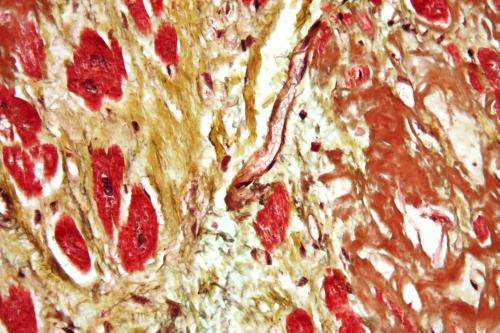
Micrograph of a heart with fibrosis (yellow) and amyloidosis (brown). Movat’s stain. Credit: Nephron/Wikipedia
New research at ACR Convergence 2023, the American College of Rheumatology’s (ACR) annual meeting, describes a link between positive antiphospholipid antibodies and an increased risk of future cardiovascular disease in patients with systemic lupus erythematosus (SLE).
Antiphospholipid antibodies (aPLs) are autoantibodies directed against phospholipid-binding proteins. In antiphospholipid syndrome, they are associated with heart attack, stroke, and pulmonary embolism, and with miscarriage and stillbirth during pregnancy.
People with SLE also have a greatly increased risk of cardiovascular disease (CVD), a major cause of morbidity and mortality in these patients. About 30 to 40% have aPLs, yet little is known about how the antibodies affect CVD risk. Suspecting they might play a pivotal role, Yufang Ding, a medical student at Peking Union Medical College Hospital, Beijing, China, and her mentors, Mengtao Li and Jiuliang Zhao, decided to explore the association between aPLs and future atherosclerotic cardiovascular disease in SLE.
For their multi-center prospective study, the researchers recruited more than 1,500 patients diagnosed with lupus between 2006 and 2021 through the Chinese SLE Treatment and Research Group (CSTAR), the largest lupus registry in China. More than 90%were women, and all were East Asian.
The team measured seven aPL isotopes at diagnosis and during follow-up:
- Anticardiolipin (aCL) antibodies
- IgG
- IgM
- IgA
- Anti-beta-2-glycoprotein I (aβ2GPI) antibodies
- IgG
- IgM
- IgA
- Lupus anticoagulant (LA), a misnomer since aPLs increase the chance of blood clots
Of included patients, 525 (33.4%) had positive aPLs. Lupus anticoagulant was the most prevalent (20.6%) followed by aCL IgG (15.8%. One hundred sixteen patients (7.37%), of whom 92 were aPL positive, developed atherosclerotic cardiovascular disease (ASCVD) during a roughly 4.5-year follow-up. Atherosclerotic cardiovascular disease was defined as a new nonfatal heart attack, nonfatal stroke, coronary or peripheral artery revascularization or cardiovascular death.
The team also conducted three analyses. The analysis concluded, first, that both aPL positivity and traditional risk factors were associated with atherosclerotic cardiovascular disease. Second, aCL IgG, aCL IgM and lupus anticoagulant were independently associated with atherosclerotic cardiovascular disease, along with smoking, hypertension and patient gender and age. Lastly, third, anticoagulant and antiplatelet therapy can reduce atherosclerotic cardiovascular disease risk in SLE patients.
Ding, the study’s lead author, says previous research has shown that an inflammatory cascade is triggered when aPLs bind to β2GPI, leading to inflammation, vasculopathy, and thrombosis, so the positive correlation between aPLs, traditional risk factors and ASCVD was expected.
But, Ding notes, “Few studies have demonstrated the role of different aPL isotopes in ACSD development. In our study, we identified that aCL IgG, aCL IgM and lupus anticoagulant positivity are independently associated with ASCVD after adjusting for traditional cardiovascular disease risk factors.”
The study has a few limitations. One, Ding says, is the “dynamic and time-varying interplay among aPL positivity,” which makes statistical analysis challenging. And because this is an observational study, it is hard to account for confounding factors like treatment choices and outcomes.
Still, Ding thinks the study results suggest that at the least, lupus patients should be tested for aPLs and those who are aPL-positive should undergo more careful surveillance for future heart disease. And, he says, “The use of low-dose aspirin for primary thrombosis prevention should be carefully considered in SLE patients with positive anticardiolipin antibodies or lupus anticoagulant. We are also looking forward to discussing the prevention role of the Mediterranean diet and exercise through an intervention study in the future.”
More information: Abstract #0552
Provided by American College of Rheumatology

Leave a Reply