By Dr. Priyom Bose, Ph.D.
Reviewed by Danielle Ellis, B.Sc.
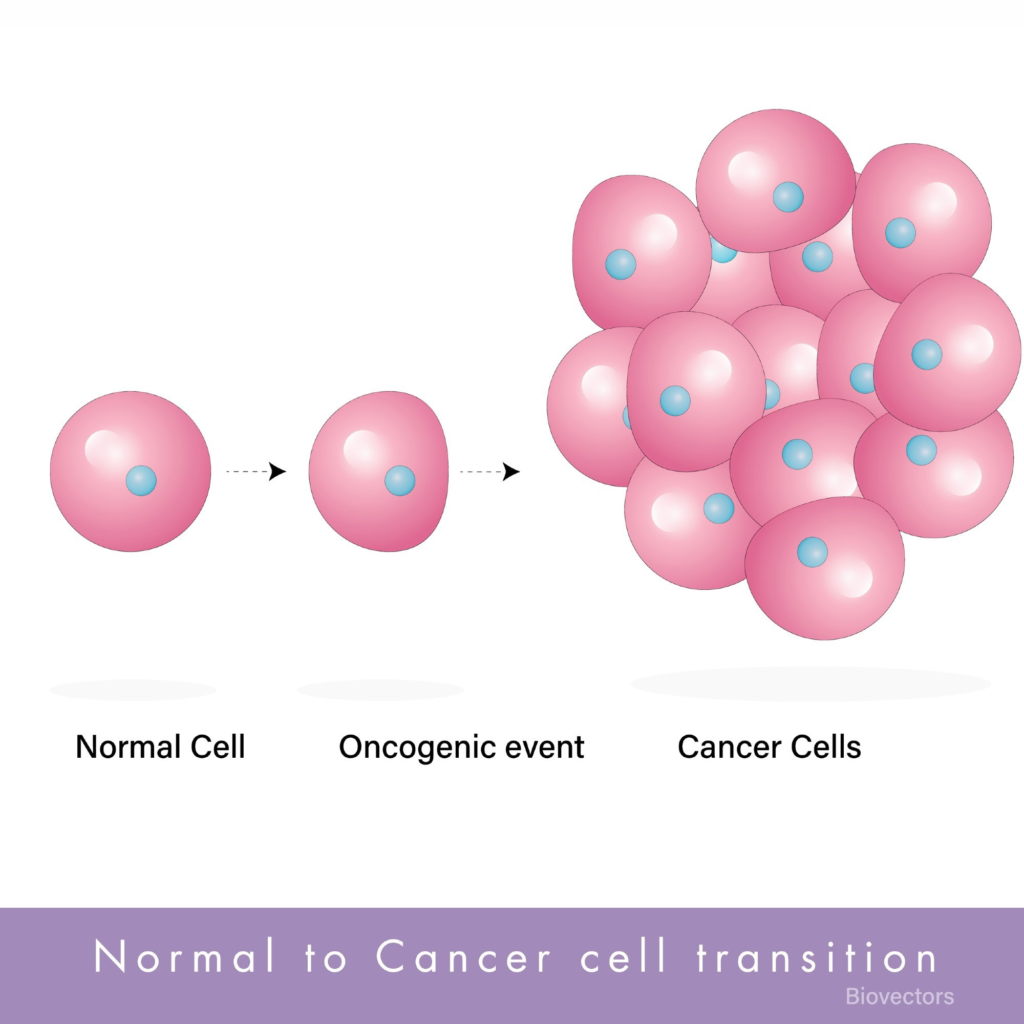
Proto-oncogenes are a group of genes that normally regulate cell division and growth by encoding regulator proteins for cell cycle, growth factors, transcription factors, DNA-binding proteins, and protein kinases that are involved in signal transduction. Upon mutation, proto-oncogenes change to oncogenes and transform normal cells into cancer cells.

Image Credit: aycan balta/Shutterstock.com
How does a proto-oncogene cause cancer?
In the early twentieth century, a tumor-causing virus called the Rous sarcoma virus (retrovirus) was discovered.3 Host cell proto-oncogene (c-src) and Rous sarcoma viral oncogene (v-src) were found to be both associated with cancer manifestation. Hybridization experiments demonstrated the presence of c-src gene in the genome of several species. Although the host cell c-src gene was found to be associated with normal regulation of cell division, the introduction of v-src oncogene through viral infection caused uncontrolled host cell growth and cell division and cancer.
Currently, more than 40 different proto-oncogenes are detected. Proto-oncogene encodes epidermal growth factor receptor (EGFR) that plays a vital role in regulating growth factor-mediated signaling. These genes also encode intracellular proteins, such as downstream signaling proteins (e.g., HRAS and KRAS), that stimulate cell growth and division.
Cyclin D1 (CCND1) and cyclin E1 (CCNE1) are proto-oncogenes that play an important role in pushing the cells to undergo distinct cell cycle stages when the cells receive the appropriate signals. However, when these genes are overexpressed, it leads to cancer.
Proto-oncogenes play an important role in embryogenesis. Generally, the activities of these genes are turned off once the developmental process they regulate is completed. In case of high proto-oncogene activity or inappropriate reactivation of proto-oncogenes later in life leads to cancer.
Proto-oncogene activation
An activated proto-oncogene by mutation or overexpression is called an oncogene. Oncogene renders the cell unresponsive to normal cell signals and ultimately leads to tumor formation. The genetic mechanisms that are involved with alteration in protooncogene structure or an elevation in protooncogene expression are mutation, chromosomal rearrangements, and gene amplification. These are briefly discussed below:
Mutation
Mutations in protooncogenes might structurally alter the encoded proteins, which might have had a regulatory role in cell division. These alterations may lead to uncontrolled and continuous activity of the protein variants. Different types of mutation, such as deletion, substitution, and insertion, can activate proto-oncogenes.
Proto-oncogene mutations are found in 15% to 20% of unselected human tumors.7 In humans, point mutations are linked with a single amino acid change within the protein, which causes tumor formation.8 This mutation type is commonly detected in the ras family of proto-oncogenes, such as H-ras, N-ras, and K-ras. The majority of ras mutations are found in codon 12 of the gene, while a smaller number is seen in codons 13 and 61.
Typically, mutations in K-ras trigger malignancy. K-ras mutations have been detected in 30% of lung adenocarcinomas, 90% of carcinomas of the pancreas, and 50% of colon carcinomas. N-ras mutations are often found in hematologic malignancies.
Gene amplification
Gene amplification is associated with an increase in copy number of a gene within a cellular genome.9 This phenomenon leads to increased gene expression, which may increase cell growth. Karyotypic abnormalities, such as double-minute chromosomes (DMs) and homogeneous staining regions (HSRs), have been associated with gene amplification due to redundant DNA replication.
Amplification of specific proto-oncogene families, such as myc, erb B, and ras, has been found in multiple human tumors. For instance, 20% to 30% of breast and ovarian cancers exhibited c-myc amplification. Furthermore, N-myc application has been robustly associated with advanced tumor stage in neuroblastoma.
Chromosomal rearrangements
Chromosomal rearrangement mainly occurs due to translocations and inversion.10 This rearrangement can cause hematologic malignancy through the transcriptional activation of proto-oncogenes. Transcriptional activation occurs when a proto-oncogene close to a T-cell receptor gene or an immunoglobulin is moved. This movement triggers the deregulation of protooncogene expression, causing the neoplastic transformation of the cell. Solid tumors, particularly sarcomas, and hematologic malignancies occur due to recurring chromosomal rearrangements.

p53: Guardian of the Genome
Therapeutic implications
Proto-oncogenes encode proteins essential for normal human development and the maintenance of organs and tissues. In contrast, oncogenes increase the production of proteins that enhance cell division, decrease cell differentiation, and inhibit apoptosis. Since these phenotypes define cancer cells, they are targeted for the development of anti-cancer interventions.
Cancers are often a multistep process during which cells acquire a series of mutations that collectively increase proto-oncogene expression and decrease tumor suppressor gene functions. Cancer cells heavily rely on oncogenic mutations for their growth, proliferation, and survival. This concept has been termed oncogene addiction.11Therefore, inhibiting the expression of a specific oncogene can effectively decrease tumor formation ability, decrease cell proliferation rate, and might increase sensitivity to chemotherapeutic agents.
How Multi-Omics Approaches Are Shaping Cancer Subtyping, Prognosis, and Diagnosis
Imatinib, an abelson murine leukemia (ABL) kinase inhibitor, has been used to treat chronic myelogenous leukemia (CML).12 This cancer type is associated with a specific chromosomal translocation that leads to a fusion protein consisting of Breakpoint Cluster Region (BCR) and ABL. After the success of imatinib, academic researchers and pharmaceutical companies have currently focused on developing therapeutics targeting oncogene activity as a treatment for cancer.
References
Newkirk KM, et al. Neoplasia and Tumor Biology. Pathologic Basis of Veterinary Disease (Sixth Edition).2007;286-321.e1. https://doi.org/10.1016/B978-0-323-35775-3.00006-0
Cooper GM. The Cell: A Molecular Approach. 2nd edition. Sunderland (MA): Sinauer Associates; 2000. Oncogenes. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9840/
Rubin H. The early history of tumor virology: Rous, RIF, and RAV. Proceedings of the National Academy of Sciences. 2011; 108(35), 14389-14396. https://doi.org/10.1073/pnas.1108655108
Chial, H. Proto-oncogenes to oncogenes to cancer. Nat Edu, 2008; 1(1):33. https://www.nature.com/scitable/topicpage/proto-oncogenes-to-oncogenes-to-cancer-883/
Simanshu DK, Nissley DV, McCormick F. RAS Proteins and Their Regulators in Human Disease. Cell. 2017;170(1):17-33. doi: 10.1016/j.cell.2017.06.009.
Alao JP. The regulation of cyclin D1 degradation: roles in cancer development and the potential for therapeutic invention. Mol Cancer. 2007;6:24. doi: 10.1186/1476-4598-6-24.
Pierotti MA, Sozzi G, Croce CM. Mechanisms of oncogene activation. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003. Available from: https://www.ncbi.nlm.nih.gov/books/NBK12538/
Liu JJ, Yu CS, Wu HW, Chang YJ, Lin CP, Lu CH. The structure-based cancer-related single amino acid variation prediction. Sci Rep. 2021;11(1):13599. doi: 10.1038/s41598-021-92793-w.
Ohshima, K., et al. Integrated analysis of gene expression and copy number identified potential cancer driver genes with amplification-dependent overexpression in 1,454 solid tumors. Scientific Reports.2017;7(1),1-13. https://doi.org/10.1038/s41598-017-00219-3
Kweon J, Hwang HY, Ryu H, Jang AH, Kim D, Kim Y. Targeted genomic translocations and inversions generated using a paired prime editing strategy. Mol Ther. 2023;31(1):249-259. doi: 10.1016/j.ymthe.2022.09.008.
Ardini, E., Magnaghi, P., Orsini, P., Galvani, A., & Menichincheri, M. Anaplastic Lymphoma Kinase: Role in specific tumours, and development of small molecule inhibitors for cancer therapy. Cancer Letters.2010; 299(2), 81-94. https://doi.org/10.1016/j.canlet.2010.09.001
Hunter T. Treatment for chronic myelogenous leukemia: the long road to imatinib. J Clin Invest. 2007 Aug;117(8):2036-43. doi: 10.1172/JCI31691.


Leave a Reply