by Gabriele Meseg-Rutzen, University of Cologne
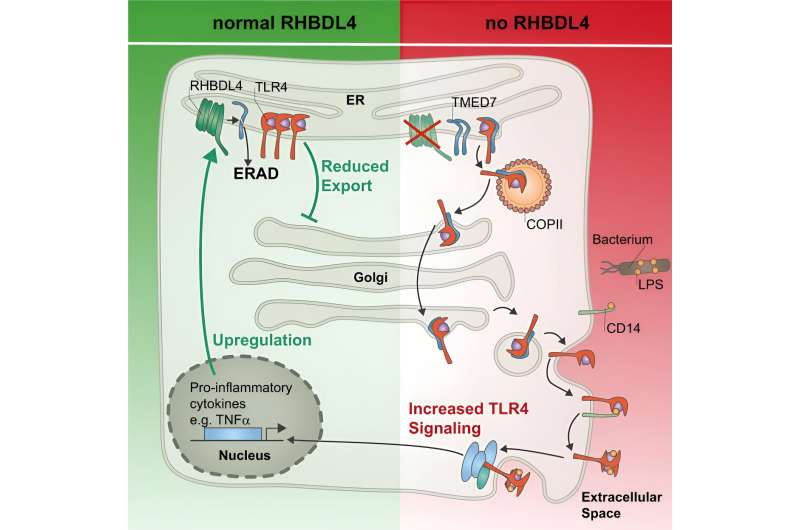
Keeping the immune system in checkModel of RHBDL4-mediated negative feedback regulation of TLR4 signaling. RHBDL4-catalyzed cleavage induces downregulation of TMED7 by the ERAD pathway. Upon loss of RHBDL4, TMED7 accumulates and promotes the trafficking of TLR4 to the cell surface. Consequently, TLR4 downstream signaling is increased, resulting in enhanced cytokine secretion. As negative feedback, LPS-induced TLR4 signaling upregulates RHBDL4 expression by an unknown mechanism. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-45615-2
Researchers from the UoC’s Center for Biochemistry at the Faculty of Medicine and the UoC CECAD Cluster of Excellence in Aging Research have discovered that an excessive immune response can be prevented by the intramembrane protease RHBDL4.
In a study now published in Nature Communications under the title “RHBDL4-triggered downregulation of COPII adaptor protein TMED7 suppresses TLR4-mediated inflammatory signaling,” the previously unknown regulatory mechanism is described.
The researchers discovered that the cleavage of a cargo receptor by a so-called intramembrane protease reduces the localization of a central immune receptor on the cell surface and thereby the risk of an overreaction of the immune system.
Intramembrane proteases are reactive proteins that reside in the cell membranes. They form a special group of proteases because they cut proteins within cellular membranes. Many of these unusual proteases have not yet been sufficiently characterized and only a few of the molecules they can cleave—the so-called substrates—and thus their functions are known.
One of these intramembrane proteases is RHBDL4. It is located in the endoplasmic reticulum, a large intracellular membrane system that is responsible, among other things, for the correct folding of newly synthesized proteins that are fed into the secretory route.
In search of substrates and RHBDL4’s molecular function, the team led by Marius Lemberg, Professor of Biochemistry and principal investigator at CECAD at the UoC, discovered a mechanism for regulating the innate immune system. This involves cleaving a transport protein and thus preventing the transport of an immune receptor to the cell surface.
In order to get a first glimpse of the physiological function of RHBDL4, the research team examined tissue culture cells for substrates using mass spectrometry. Among the substrate candidates were several so-called cargo receptors. These are proteins that are necessary for the transport of specific proteins along the secretory route.
Contrary to what has long been assumed, most proteins are not simply secreted from the endoplasmic reticulum in a non-specific manner, but must be selected and transported by cargo receptors. One such cargo receptor, TMED7, has now been characterized as a substrate of RHBDL4.
By cleaving this cargo receptor, the cell can precisely and quickly control the transport of certain proteins and thereby adapt the cell to the given environmental conditions. “This type of regulation of transport processes by cleavage of cargo receptors by an intramembrane protease has not yet been described,” said Lemberg.
This finding is particularly interesting in light of the fact that the cargo receptor TMED7 transports a central immune receptor of the body’s innate immune system to the cell surface—the so-called toll-like receptor 4 (TLR4). When TLR4 comes into contact with components of bacterial cell walls, it induces an immune response, i.e., a defense reaction. Cleavage of the cargo receptor TMED7 by RHBDL4 results in fewer TLR4 molecules reaching the cell surface and consequently in a reduction of the immune response to bacterial cell wall components.
Since overactivation of TLR4 can harm the organism and even contribute to blood poisoning (sepsis), the TLR4-mediated immune response must be strictly regulated by the body. Using a mouse model, the team demonstrated in collaboration with Dr. Colin Adrain of Queen’s University Belfast, U.K., that RHBDL4 is crucial to prevent overactivation of TLR4. This protects the organism.
“When the receptor is stimulated, cells produce more RHBDL4—this is why there is a negative feedback loop that prevents an excessive immune response by the receptor from harming the organism,” said Lemberg.
In order to learn more about the clinical relevance of transport regulation by RHBDL4, the team collaborated with the group of Dr. Jan Rybniker at University Hospital Cologne and discovered that the regulation is also important when cells are exposed to pathogens such as the tuberculosis germ Mycobacterium tuberculosis.
In addition, the team led by Professor Lemberg linked a genetic mutation in the protease RHBDL4 to the Kawasaki syndrome, which is an immunological disease associated with an overreaction of the immune system that particularly affects children.
“This project shows the power of basic research using very simple models such as tissue culture cells to gain fundamental new insights into human biology and disease,” concluded Lemberg.
More information: Julia D. Knopf et al, RHBDL4-triggered downregulation of COPII adaptor protein TMED7 suppresses TLR4-mediated inflammatory signaling, Nature Communications (2024). DOI: 10.1038/s41467-024-45615-2
Journal information: Nature Communications
Provided by University of Cologne

Leave a Reply