by Kitta MacPherson, Rutgers University
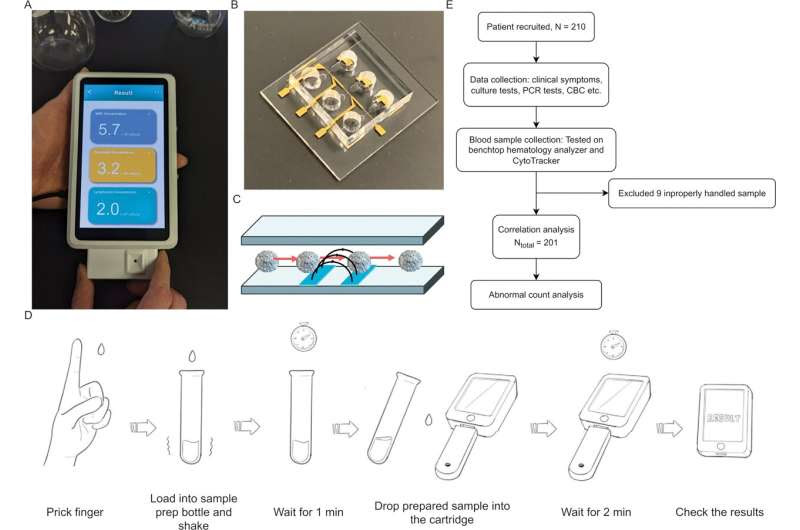
Study overview. (A) Image of CytoTracker device prototype. (B) An image of the CytoTracker microfluidic impedance cytometer. (C) Schematic of sensing mechanism. (D) A diagram of the proposed user workflow. Drop of blood is obtained from patient, then placed into sample processing tube for lysis of red blood cells. After waiting for one minute, several drops of processed blood are squeezed into the test strip (plugged into device). After waiting for two minutes, the result is available for the user. (E) An overview of study workflow. 210 adult patients with symptoms were recruited. Nine patients were excluded due to the sample being improperly handled during shipment. As a result, the final analysis was obtained from 201 patients. Credit: PLOS ONE (2024). DOI: 10.1371/journal.pone.0296344A Rutgers researcher, through his spinoff company, has led a team to design and test a device that quickly counts a person’s white blood cells with a single drop of blood, similar to the way glucometers rapidly scan for blood sugar levels.The development of the device by researchers at Rutgers startup RizLab Health Inc., along with the clinical validation, is described in the science and medical journal PLoS One.Mehdi Javanmard, a professor in the Department of Electrical and Computer Engineering in the Rutgers School of Engineering, is the co-founder and CEO of RizLab Health Inc, based in Princeton. He launched the startup based on advances in his Rutgers lab.”Normally, doing a blood count requires a phlebotomist taking a needle stick and collecting significant amounts of venous blood and sending the samples off to labs where they are tested, sometimes taking hours or even days,” Javanmard said. “Our handheld device enables near-patient testing, while only requiring a tiny amount of blood and returning results within minutes, allowing clinicians to make decisions almost immediately.”Called the CytoTracker Leukometer, the device is designed to quickly aid the detection of elevated or reduced white blood cell counts, a critical signal of a patient’s immune system status. A high or low white blood cell count may indicate the intensity of an infection, the presence of life-threatening conditions such as sepsis or determine how patients are responding to chemotherapy and psychotropic drugs.In collaboration with a clinical team at the Rutgers Robert Wood Johnson Medical School Pediatric Clinical Research Center led by Dr. Tanaya Bhowmick and the Baylor College of Medicine Department of Emergency Medicine, the device was successfully tested in trials via a direct comparison with a lab benchtop hematology analyzer, a conventional blood testing technique.”Rapid test results have revolutionized the field of medicine,” said Bhowmick, an infectious disease physician and co-author of the paper. “The white blood count is a parameter that physicians routinely order to evaluate a patient for possible infection. Having this information rapidly can help triage patients in the outpatient setting.”The results showed the CytoTracker Leukometer to be at least 97% accurate and to meet clinical standards.White blood cells, or leukocytes, protect the body from infection. Colorless, they constitute about 1% of human blood and are formed mostly in the bone marrow. Certain subtypes of leukocytes have different functions. For example, neutrophils kill bacteria, fungi and foreign debris.A low white blood cell count indicates that a person is prone to infection. A high white blood cell count means either an infection exists or there is an underlying medical condition.Javanmard said he envisions multiple uses for the device. Sepsis in a patient entering an emergency room could more quickly be detected on the device than through present methods requiring a blood draw and a lab test, he said. Cancer doctors could rapidly determine whether patients undergoing chemotherapy need a white blood cell stimulant.The device also may make it easier for psychiatry patients to stay on their medications. Patients taking clozapine, a common treatment for disorders such as schizophrenia, often experience neutropenia, or low levels of neutrophils. These patients are required to undergo regular testing for neutrophil levels before they can obtain a prescription. Javanmard said this often prevents patients from procuring much-needed treatment.In his Rutgers lab, Javanmard and his students have sought to perfect the capabilities of a miniaturized electronic cytometric technique that detects microscopic particles by directing them through minute channels containing electrodes. The process is akin to scanning people as they move individually through an airport security gate; however, it uses electrical signals instead of videography.In one recent advance, Javanmard said he and lab members used the cell-flow technique to develop a test so sensitive it could someday revolutionize medical approaches to epidemics. RizLab Health has focused on further advanced development and manufacturing of electronic cytometry with the goal of obtaining regulatory approval and ultimately commercialization.Javanmard is excited about applying lab insights to practical problems to produce inventions like the CytoTracker Leukometer.”We set out to solve one of the holy grails of medicine, which is to analyze a tiny amount of a patient’s blood in a way to give guidance to clinicians and improve clinical outcomes,” Javanmard said. “We believe this will have a huge impact in infectious disease, oncology, and psychiatry.”Javanmard added, “Others have made failed attempts to tackle this holy grail by aiming to identify dozens or even hundreds of biochemical constituents with a single drop of blood. Such attempts are fundamentally very difficult. As a result, we found it to be much more realistic to focus only on the white blood cells with the key sub-types as a start.”The device must be approved by the Food and Drug Administration before it can be commercialized and used for clinical applications, Javanmard said. It is presently for research use only.Other scientists on the paper from Rutgers included Fei Chen, a staff nurse at the Rutgers Robert Wood Johnson Medical School Pediatric Clinical Research Center, and Sunanda Gaur, a pediatric infectious disease physician and director of the medical school’s Pediatric Clinical Research Center. Scientists at Baylor included Kelly Keene, Farzad Soleimani and Zubaid Rafique.More information: Jianye Sui et al, Clinical evaluation of a fully electronic microfluidic white blood cell analyzer, PLOS ONE (2024). DOI: 10.1371/journal.pone.0296344Journal information: PLoS ONE Provided by Rutgers University

Leave a Reply