by The University of Hong Kong
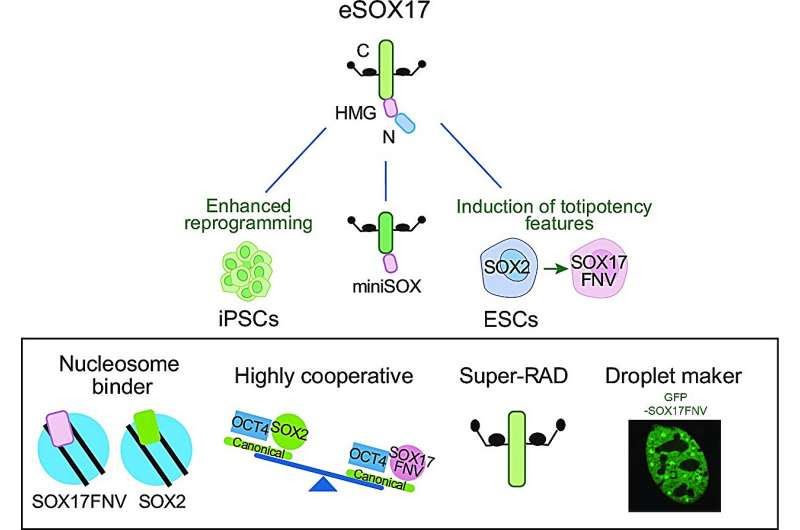
Credit: Nucleic Acids Research (2023). DOI: 10.1093/nar/gkad597
A research team from the School of Biomedical Sciences, LKS Faculty of Medicine of the University of Hong Kong (HKUMed), has achieved a breakthrough in stem cell research, offering tools that can be used for patients who require highly personalized care.
The team has developed an innovative method to transform blood and skin cells into neural stem cells, overcoming the limitations of current stem cell research techniques while opening up new possibilities for studying and working toward treatments for age-related diseases, such as Alzheimer’s, Parkinson’s, and Amyotrophic lateral sclerosis.
The findings are published in Science Advances and Nucleic Acids Research.
The human body consists of approximately 200 different cell types, each playing a critical role in maintaining overall health. However, accessing and analyzing certain cell types, such as neurons located deep within the brain, have been challenging.
The conventional approach to generating induced pluripotent stem cells (iPS cells) involves using easily accessible cell sources, such as skin, blood, and urine. These iPS cells have similar characteristics to pluripotent stem cells found in early embryos and can be differentiated into various cell types, including those found in the brain, heart, liver, and lungs.
However, creating iPS cells is time-consuming, costly, and often associated with safety concerns, since iPS cells have some similarities to cancer cells. In addition, iPS cells represent a young embryonic state, so they are typically unsuitable for studying age-linked diseases.
In response to these challenges, Professor Ralf Jauch, Associate Professor, the School of Biomedical Sciences, HKUMed, and his team have been actively exploring innovative solutions to overcome these limitations.
Professor Ralf Jauch (centre), the School of Biomedical Sciences, HKUMed, and his research team have developed an innovative method to transform blood and skin cells into neural stem cells, overcoming limitations of current stem cell research techniques which will help enhance the understanding and treatment for age-related diseases. Credit: The University of Hong Kong
Early attempts at inducing neural stem cells were slow and ineffective, relying on natural genes present in the human genome, such as SOX2. The team took advantage of a powerful molecule, called SOX17, which is a distinct relative of SOX2 and typically functions in blood, gut and lung cells. The team transformed SOX17 into a “super stem cell factor” through mutations. The mutant variant of SOX17 exhibited an improved capability to activate silent genes, self-organize within the nucleus, and navigate from gene to gene with precision, resulting in rapid and efficient cell transformation.
The researchers successfully transformed skin cells from mice of different ages into neural stem cells that possess the characteristics of brain-residing cells. They further refined this methodology for human cells, enabling the conversion of blood cells from human donors into neural stem cells that could be further differentiated into the specific cell types associated with motor neuron diseases or dementia.
The team also identified crucial features of the mutant SOX17 and developed a miniSOX variant which reduced the packaging load required for delivery to target cells or organs. This discovery explains the importance of using tailor-made SOX proteins for the successful conversion of skin and blood cells into neural stem cells. A non-provisional patent application on the use of engineered SOX17 has been filed for the development of the next-generation of stem cell models.
Traditional embryonic stem cells and iPS cells often fail to fully capture the characteristics of aging cells, limiting their utility in studying and addressing age-related diseases. The team has successfully preserved aging features in stem cells derived from mice, providing a more authentic system for studying age-related diseases and exploring potential treatments. The next phase of their research involves studying neural cells generated from the blood cells of older humans to validate these findings.
This groundbreaking research, led by Professor Jauch, holds promise in the realm of regenerative medicine and personalized patient care. “The shortcut of generating neural stem cells from easily accessible sources could provide a faster, more cost-effective, and safer way to generate next-generation stem cells, opening the doors to understanding and treating a wide range of diseases associated with aging,” said Professor Jauch.
“These findings represent a significant milestone in the field of stem cell research. Leveraging the potential of stem cells, we can begin to unlock personalized treatment strategies, tailored to the unique needs of individual patients,” Professor Jauch added.
Provided by The University of Hong Kong

Leave a Reply