by Sylvester Comprehensive Cancer Center
Credit: Unsplash/CC0 Public Domain
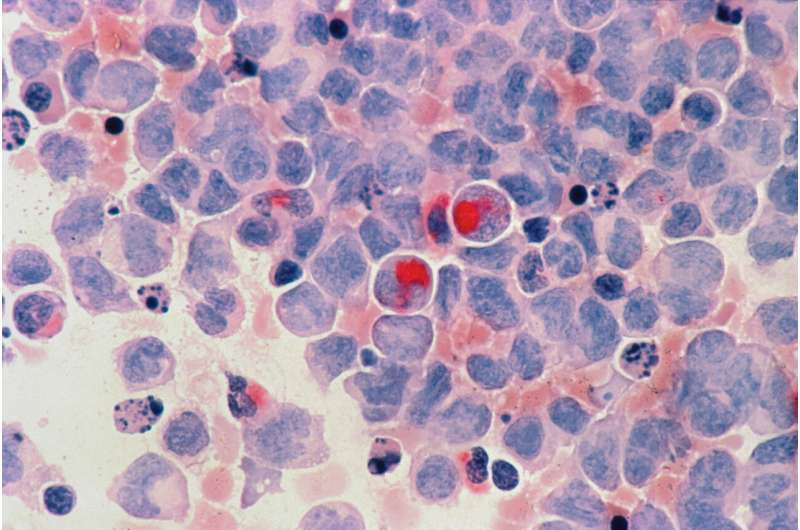
Researchers have shown for the first time exactly how immature neutrophils—white blood cells that are an important part of the immune system—are hijacked by pancreatic cancers to drive immunosuppression and treatment resistance. The study, led by investigators at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine, is published in Cancer Discovery, a journal of the American Association for Cancer Research.
The paper describes a previously unrecognized signaling circuit in pancreatic cancer that instigates immunosuppression and tumor-promoting inflammation in the pancreatic tumor microenvironment, ultimately creating treatment resistance. The central regulator of this treatment resistance is neutrophil-derived TNF signaling. TNF, or tumor necrosis factor, is a substance in the body that causes inflammation.
This is the first study to implicate immunosuppressive signaling from immature neutrophils—the earliest sentinels in developing pancreatic cancer—in this process, said Jashodeep Datta, M.D., associate director of Translational Research at the Sylvester Pancreatic Cancer Research Institute. Datta, whose laboratory at Sylvester led the research, is senior author of the multicenter study.
“It suggests neutrophils are a dominant actor in this circuit. This is the first description of how cancer cells talk with neutrophils and how neutrophils are major actors in this immunosuppressive inflammatory drama in the pancreatic tumor microenvironment,” said Datta, the DiMare Family Chair in Immunotherapy at the Miller School.
He said the research is critical to scientists’ knowledge of pancreatic cancer—one of the most treatment-resistant cancers—because it “connects the molecular dots between the high-risk tumor genotypes that exist in pancreatic cancer and the specific molecular and cellular culprits—the immature neutrophils—that are involved in creating immunosuppressive networks in the pancreatic tumor microenvironment.” The research team, Datta said, is “creating a road map to target each element of these molecular dots” to thwart this inflammatory process and overcome therapeutic resistance.
Nipun Merchant, M.D., the founding director of the Sylvester Pancreatic Cancer Research Institute and a co-author of the paper, said the research “will pave the way to the ultimate goal of clinical studies, so that our findings can be directly translated to improve patient care.”
Datta said clinical trials will attempt to target the immunosuppressive pathway from numerous angles.
“We’re collaborating with multiple groups across the country to make this happen and are developing a novel nanoengineering platform to target neutrophils without killing them so we can target the tolerogenic [immunosuppressive] signaling mechanisms within neutrophils,” he said.
To make the discovery, the Sylvester team collaborated with researchers in different disciplines at the Miller School, including the departments of Microbiology and Immunology, the Diabetes Research Institute, and Public Health Sciences. They also worked with colleagues at other medical schools and cancer centers, including Johns Hopkins, the University of Pennsylvania, and Harvard.
The researchers leveraged cutting-edge technologies, including single-cell biology, where they used spatial techniques to understand cellular relationships in the pancreatic tumor microenvironment. They used high-dimensional sequencing to understand how cancer cellsand neutrophils orchestrate this crosstalk.
They brought it all together with mechanistic and translational studies using certain drugs to overcome chemotherapy resistance in cellular and animal models, as well as by using blood samples and tissue specimens made available by patients at Sylvester.

Leave a Reply