by Stony Brook University
As the COVID-19 pandemic spreads and nears its so-called apex in New York State, the need for N95 respirator masks, which protect against inhalation of airborne coronavirus molecular particles, is still a top concern. According to new research being conducted at the Stony Brook University MART building, dry heat ovens have been shown to be effective for disinfecting N95 masks.
Led by Kenneth R. Shroyer, MD, Ph.D., The Marvin Kuschner Professor and Chair of the Department of Pathology and a team that includes Glen Itzkowitz, Associate Dean for Research Facilities & Operations and graduate students Sruthi Babu and John Yuen, the team conducted pilot studies to determine if N95 masks were degraded after multiple rounds of dry heat treatment.
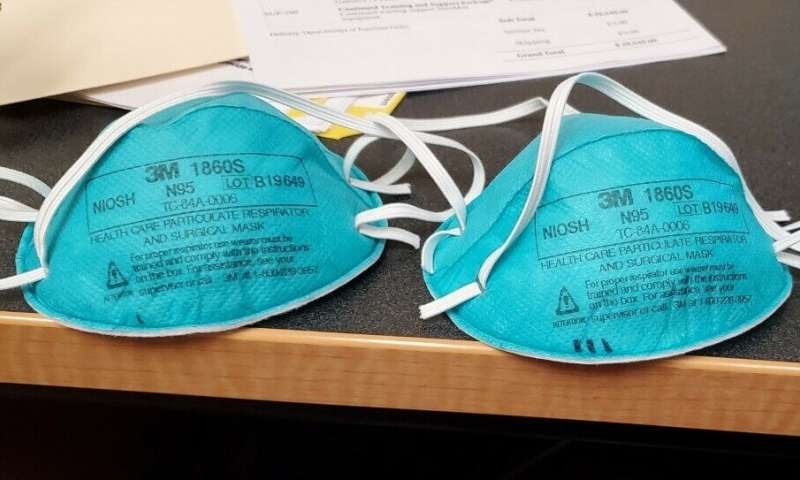
Through the studies, they found that particularly 3M N95 masks passed quantitative “fit-tests,” the industry standard to ensure protection against coronavirus inhalation after multiple rounds of dry heat treatment. The heat-treatment caused no visible structural damage and had no effect on the straps required to ensure proper fit, the study showed.
“Fit test scores were virtually identical between masks processed through four repeated cycles, suggesting that this approach could effectively increase the usable supply of N95 masks by a factor of five,” said Dr. Shroyer. “It appears that the heat treatment can also be used to treat other types of surgical facemasks.”
This study was completed in a high capacity oven that could process thousands of masks per day, concluded the team. Yet, they said, “equivalent results could be achieved at most hospitals, clinics, or nursing homes following a similar protocol in any conventional dry heat oven or incubator.”
About the Protocol
Healthcare providers place a used 3M respirator mask in a paper bag labeled with their name and work location before delivery to the processing center. The bags containing the masks are then sealed with heat indicator tape before they are placed in the oven. Following treatment for 30 minutes at 100˚C (212˚F)*, the same bags can then be returned to the clinical care providers.
Dr. Shroyer and colleagues concluded that heat treatment of N95 could be used at health care facilities that have no other viable options. It could provide a better alternative approach, recently recommended by the CDC, that both the general public and health care providers should utilize bandanas or scarves once supplies of facemasks are depleted. Additionally, dry heat disinfection may be more readily available during the pandemic than hydrogen peroxide vapor generators. Although, according to Itzkowitz, a combination of vapor decontamination and dry heat decontamination would make for the best results.
“The team has discussed potential fabrication efforts to construct a sterilizer racking system capable of recycling as many as 8,000 masks a day through the heat treatment,” said Itzkowitz. “As many as eight institutions have already indicated that they may start using this technique for PPE recycling following COVID-19 exposure.”
Glen Itzkowitz discusses what led to the new approach
I came into the project after autoclaving sanitization was attempted and determined to be a nonstarter. This had followed an email discussion about Vaporized Hydrogen Peroxide solution the night before. We believe the autoclave failed due to the fact that when that equipment pulled vacuum and then heated up, the 1860 model masks would become deformed.
Think of an autoclave as a big pressure cooker. These masks failed fit testing by Environmental Health & Safety (EH&S). Ken [co-PI Dr. Ken Shroyer] and I were talking about this and I told him about the dry heat sterilizer technology we installed in the MART DLAR satellite facility cage wash on MART level 3. This technology was selected over a bulk autoclave because of steam pressure limitations in that part of the MART.
Dry heat sterilizers are not pressurized vessels, they do not use vacuum as part of their process. We agreed to give this equipment a shot. The satellite vivarium (a place, such as a laboratory, where live animals or plants are kept under conditions simulating their natural environment, as for research) in the MART is not yet active so the equipment in this cage wash facility other than being installed at this time, had not been used yet. Ken’s team determined soak cycles and tested a variety of PPE at different temperatures as well as lengths of cycles, temperature set point deviations, and ramp down time cycles.
The initial testing on the 1860 model was at 250F (121C) for a duration of 60 minutes with a 30 minute ramp down and a 5C degree deviation. These masks failed the qualitative fit test by EH&S following this soak. We then decided that temps were likely higher than they needed to be and cycles were too long. The next attempt used 1870 model N95s at 250 for 60 minutes. These masks passed. The 1870 model is a soft frame N95, it is the less commonly used mask in healthcare compared to the 1860 rigid frame model).
We started a discussion with the equipment manufacturer, TPS Gruenberg, and asked them what they knew of similar studies and efforts. They offered to come to our site to spike thermal data collection probes into the masks and retest. We ran another test on five 1870 masks with the engineer from TPS and got some very interesting data. It is also interesting to note that a bacterial biological thermal indicator was placed into the masks run in this test by Ken’s lab. The bio indicators were all color changed following the soak at 250F. This indicates a positive 6 log kill (a log reduction or “kill” means the amount, by percentage, of biological material is 10 times smaller than a given starting point. Therefore, 6 log means that 99.9999% of the biological material is killed). 6 log is needed to claim disinfection.
Because the TPS Gruenberg equipment works by convection heat with a HEPA filtered exhaust, there is a natural cooler location in the chamber itself. Hence, this part of the chamber will take longer to heat up to the desired set point. Having located the “cool” corner of the chamber through the test we ran on sight with the TPS engineer, we made some really informed decisions for retesting the 1860 model.
We knew we were onto something when TPS asked us to speak on a conference call they were organizing about using this platform for PPE recycling following COVID19 exposure. There were about eight other institutions on that call.
Following that, Ken and I reviewed the previous cycles and determined the appropriate recipe for sterilization. We layered that over what we learned from analyzing TPS’ data logger test. The result was the following change to the protocol:
Cut the duration of the cycle soak time because we understood where the chamber was more efficient.
Test in places in the chamber where the heat gradient is more uniform.
Reduce the set point temperature to 100C and achieve a 6 log kill of the virus (COVID19) on the mask based on other Coronavirus literature that Ken has been reviewing.
Use a sealed lighter weight paper autoclave bag because the temperature was now lower than previous tests.
Secure the bag to the rack frame so that they would not be moved out of place by the convection fan internal to the equipment. Thereby attempting to keep all things uniform during the testing.
We also discussed fabrication efforts to construct a truck (sterilizer racking system) that would be capable of heating approximately 1,000 N95’s per 30 minute cycle. Hence in an eight-hour day recycling as many as 8,000 masks.
One other consideration that we had discussed: our equipment is HEPA (High Efficiently Particulate Air) Filter equipped. This is very important in a convection heat sterilizer. It ensures that if any aerosolized virus particles escape the sealed autoclave bags are filter trapped during soak and killed as the filter heats up as well.

Leave a Reply