by Daniel Meierhans, ETH Zurich
The DEGs we identified upon 2 h, and 18 h of DEX treatments in A549 cells align with the other existing RNAseq and ChIP-seq datasets. Credit: Nature Communications (2023). DOI: 10.1038/s41467-023-44031-2
Stress isn’t merely an oppressive feeling we experience when we’re overwhelmed; it’s the body’s natural reaction to acute or persistent strain. This stress response is what enables us to quickly adapt to danger or a shift in conditions. But if this response—which is essential for survival—gets out of control and becomes a permanent state, it can trigger a wide range of negative effects: obesity, cardiovascular diseases, increased susceptibility to infection, memory disorders and depression are all typical effects of chronic stress.
Up to now, medical treatment has focused almost entirely on the symptoms of these secondary conditions. “The only approved drug that directly intervenes in the regulation of stress responses has a host of unwanted side effects. It was actually developed as an abortifacient and its impact on stress is merely a side effect,” explains Katharina Gapp, head of the Epigenetics and Neuroendocrinology group at the Institute for Neuroscience at ETH Zurich.
In collaboration with three other ETH research groups, Gapp has now developed a promising new agent that pinpoints and eliminates the control center of the stress response—what’s called the glucocorticoid receptor—in cell cultures and animal models. In the future, this could enable stress-related conditions such as chronic depression to be treated much more specifically and with fewer side effects. The study is published in Nature Communications.
Receptor is key to cortisol’s efficacy
By eliminating the receptor protein, the researchers are preventing the stress hormone cortisol from triggering the reaction in the first place. This is because in order to activate the genes responsible for the stress response, cortisol must bond with the glucocorticoid receptor. That’s when the body experiences the typical symptoms of stress such as elevated pulse rate, increased blood flow to muscles, a surge in metabolic activity, decreased pain perception and heightened concentration.
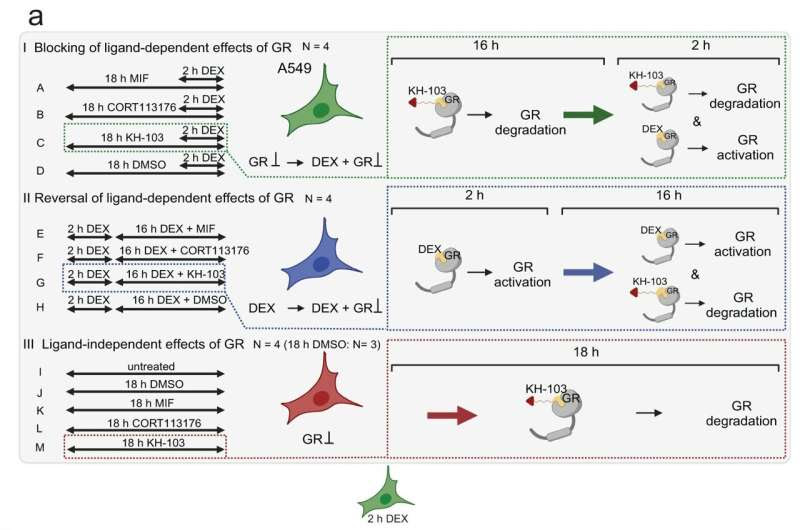
In contrast to the above-mentioned abortifacient drug, the new ETH molecule essentially affects only the glucocorticoid receptor. This is thanks to what’s known as the proteolysis-targeting chimera (PROTAC) method, which allows the agent to target the receptor proteins and supply the cells with a natural degradation system.
The right configuration of receptor and enzyme
PROTAC drug molecules are made up of two different functional subunits that share a connection. One of the two subunits binds specifically to an enzyme, which chemically tags the proteins in the cell that are to be degraded. The second subunit is designed to bind as selectively as possible to the protein of interest (POI) targeted for deactivation. By bringing the enzyme and POI in close proximity to one another, the drug molecule ensures the protein gets tagged and thus degraded.
As elegant the method is in theory, it’s actually really difficult to achieve in the lab. Getting the selective tagging of the glucocorticoid receptor to work depends on ensuring that the two functional subunits bind in as targeted way as possible to the tagging enzyme and the receptor. In addition, the length and type of connection between the two subunits must exactly match the specific enzyme-protein pairing.
Organic chemistry, bioengineering and molecular neurosciences
Designing, synthesizing and fully testing potential PROTAC agents calls for specialized know-how from a wide variety of disciplines. Gapp was able to count on the expertise of three ETH research groups: Erick Carreira’s team of organic chemists designed and synthesized the molecule variants, Andreas Hierlemann’s group at the Bio Engineering Laboratory carried out measurements in cell systems, and members of the Molecular and Behavioral Neuroscience group led by Johannes Bohacek helped test the effects in mice.
“As the project went on, it got larger and more complex,” Gapp recalls. “The collaboration with leading specialists from such varied disciplines was essential for success. ETH provides the ideal framework for this kind of endeavor.”
Next steps towards creating a drug
As they move towards creating a drug, the scientists now need to understand exactly how the molecule operates in the cells, its dose/effect relationships, how it interacts with other molecules, and how it is absorbed, dispersed and metabolized by the body. Even if all goes well, it will still be at least several years before the first applications are ready for patients.
Gapp is convinced that the PROTAC method holds vast potential for creating new drugs. “Unlike existing agents, which are capable of blocking only one receptor each, a single PROTAC molecule is able to tag a great many POIs, one after the other,” Gap said. As such, the doses required—and thus the number of potential side effects—are low.
More information: Mahshid Gazorpak et al, Harnessing PROTAC technology to combat stress hormone receptor activation, Nature Communications (2023). DOI: 10.1038/s41467-023-44031-2
Journal information: Nature Communications
Provided by ETH Zurich

Leave a Reply