Ewen Callaway
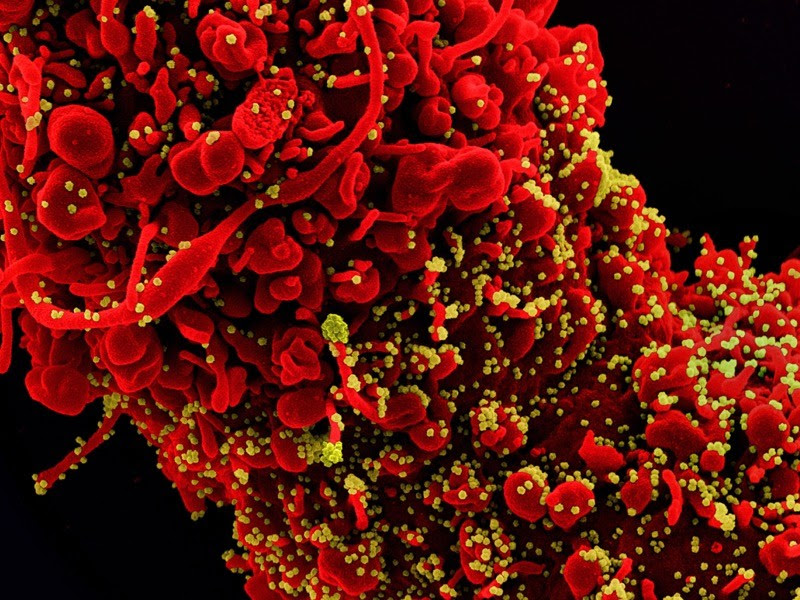
A cell (red) infected with SARS-CoV-2 particles (green).Credit: NIAID/NIH/SPL
Researchers developing the Oxford–AstraZeneca COVID-19 vaccine have identified biomarkers that can help to predict whether someone will be protected by the jab they receive.
The team at the University of Oxford, UK, identified a ‘correlate of protection from the immune responses of trial participants — the first found by any COVID-19 vaccine developer. Identifying such blood markers, scientists say, will improve existing vaccines and speed the development of new ones by reducing the need for costly large-scale efficacy trials.
“We would like to have an antibody measure that is a reliable guide to protection because it could speed up the licensure of new vaccines,” says David Goldblatt, a vaccinologist at University College London.
New formulations of influenza vaccines, for instance, are generally judged by whether they trigger a strong enough antibody response against a viral protein in a relatively small number of people, instead of in large trials that look for reductions in rates of infection. Researchers and regulators hope to do the same with COVID-19 vaccines.
“The power of a correlate in vaccines is profound,” says Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston, Massachusetts. “If there’s a reliable correlate, then it can be used in clinical trials to make decisions as to what vaccines are likely to work, what form of vaccines are likely to work, or how durable the vaccines are going to be.”
The findings are reported in a preprint study posted to medRxiv on 24 June1.
Searching for markers
Correlates of protection is typically determined by comparing the immune responses of trial participants who were protected by a vaccine to those of ‘breakthrough cases’ — volunteers who got a vaccine but still became infected.
But owing to the high efficacy of many COVID-19 vaccines, it has taken longer than expected for developers to determine markers of vaccine protection on the basis of breakthrough cases, says Peter Dull, deputy director for Integrated Clinical Vaccine Development at the Bill & Melinda Gates Foundation in Seattle, Washington.
In the absence of studies of breakthrough cases, several teams have attempted to determine a correlate of protection for COVID-19 vaccines by comparing published data on vaccine efficacy with those from earlier trials measuring immune responses to the jabs2.
These studies suggest that virus-blocking ‘neutralizing’ antibodies are a good predictor of a vaccine’s success. Those that trigger high levels of these antibodies, such as the Pfizer–BioNTech and Moderna jabs, are more effective than the Oxford–AstraZeneca and Johnson & Johnson vaccines, which generated relatively low levels of neutralizing antibodies.
The Oxford–AstraZeneca study confirms the relationship between higher neutralizing-antibody levels and protection. The analysis, led by Oxford biostatistician Merryn Voysey, compared the immune responses in 171 breakthrough cases with those of more than 1,404 people who got the vaccine and did not develop an asymptomatic infection.
Participants who had higher levels of neutralizing antibodies — as well as ‘binding’ antibodies, which recognize the SARS-CoV-2 spike protein — tended to gain stronger, but not total, protection from asymptomatic infection, the Oxford team determined. The team used a model to estimate the antibody levels that corresponded to different levels of vaccine protection against COVID-19 in trials, ranging from 50% to 90% protection. Other vaccines that trigger similar antibody responses can be expected to generate similar levels of protection against symptomatic infections, the Oxford team says.
Miles Davenport, an immunologist at the University of New South Wales in Sydney, Australia, notes that there was no significant difference in the neutralizing antibody responses of breakthrough infections and controls. This could occur if young people at greater risk of infection — because they have more social contacts, for example — also had higher antibody levels. The Oxford team accounted for this overlap in their model by estimating participants’ risk of infection. However, Davenport says that it’s a challenge to identify protective antibody levels based on estimated risk, rather than observed differences in antibody levels — which would have been possible only if there were clear differences between breakthroughs and controls.

Researchers developing the Oxford–AstraZeneca vaccine say the biomarkers they identified can help to predict whether someone will be protected by the jab they receive.Credit: Cristian Leyva/NurPhoto/Getty
It’s not certain whether the antibody levels established in the study will be able to predict the success of other vaccines, Goldblatt says, particularly those based on different technologies. “We don’t want to develop something just for one vaccine or one kind of vaccine,” says Goldblatt. “We’ve got all these manufacturers around the world, developing vaccines based on different platforms.”
The Oxford vaccine uses a harmless chimpanzee adenovirus to instruct cells to make the SARS-CoV-2 spike protein, whereas those developed by Moderna and Pfizer–BioNTech use RNA molecules to do this. Other COVID-19 vaccines deliver the protein itself or inactivated versions of the entire SARS-CoV-2 virus.
Another team is working out correlates of protection for vaccines supported by the US government, including those from Moderna and Johnson & Johnson. The Moderna analysis is expected soon.
Predicting protection
Philip Dormitzer, vice-president and chief scientific officer of viral vaccines at Pfizer, says it’s not clear whether the high levels of neutralizing antibodies explain the protection the company’s vaccine offers. Their levels are undetectable in most people before they receive a second dose, but clinical trials and real-world studies suggest that the vaccine offers strong protection after one dose. Neutralizing antibodies also do a poor job at predicting vaccine efficacy against variants, he says, and their levels wane over time.
Dormitizer and other researchers say it’s important to distinguish between biomarkers that can simply predict the success of vaccines and those that are responsible for their protective effects. In addition to neutralizing antibodies that block infection in laboratory assays, vaccines trigger antibodies with other properties, as well as T cells that kill off infected cells and support other immune responses. All of these parts of the immune response could have a role in protection.
Ultimately, it will be up to regulators to decide how to apply correlates of protection for COVID-19 vaccines, says Dull. This is already starting to happen. The UK’s medicines regulator has signaled that it could approve a vaccine using inactivated SARS-CoV-2, developed by French biotech company Valneva if it triggers higher levels of antibodies than does the Oxford–AstraZeneca vaccine in a trial of 4,000 participants.
Dull says it’s important to move carefully when determining and applying correlates of protection to COVID-19 vaccines. If vaccines approved on the basis of a biomarker turn out to perform poorly in the real world, it could undermine immunization efforts. But he hopes that developers, regulators, and stakeholders can soon settle on some answers. “We are in an era where there is limited capacity to run new efficacy studies,” he says. “Let’s get some more vaccines moving forward.”

Leave a Reply