by Weill Cornell Medical College
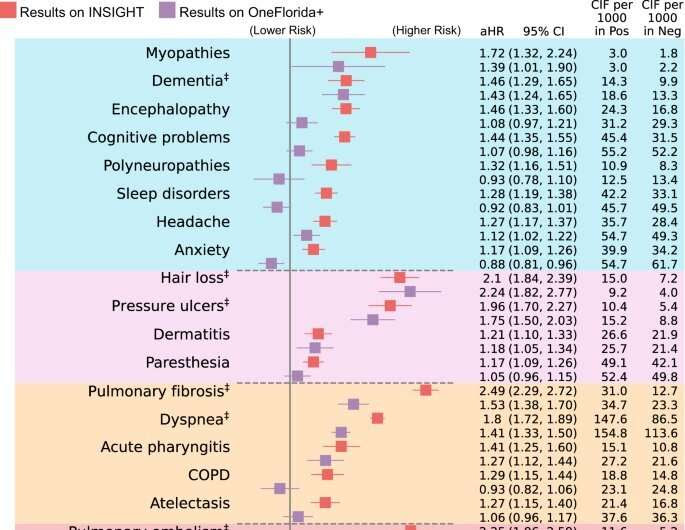
Comparison of the PASC risks in the INSIGHT cohort versus in the OneFlorida+ cohort, from March 2020 to November 2021. The incident risk was measured by the adjusted hazard ratios (aHR) with 95% confidence intervals as shown in the main panel. The adjusted cumulative incidences (CIF) per 1000 patients in both the SARS-CoV-2 positive group and the negative group were also reported. The PASC conditions identified in both datasets were marked by ‡ symbols. The color panels represent different organ systems, including (from top to bottom): the nervous system, skin, respiratory system, circulatory system, endocrine and metabolic, digestive system, genitourinary system, and other signs. The PASC outcomes were ascertained from day 30 after the SARS-CoV-2 infection and all the adjusted risk measures were computed 180 days after the SARS-CoV-2 infection. The aHRs of PASC diagnosis code U099/B948 were not illustrated here. COPD, Chronic obstructive pulmonary disease. PASC, post-acute sequelae of SARS-CoV-2 infection. Credit: Nature Communications (2023). DOI: 10.1038/s41467-023-37653-z
While the peak of the COVID-19 pandemic seems to have passed, the effects of post-COVID conditions on public health remain. A new study led by Weill Cornell Medicine and NewYork-Presbyterian investigators has found that the risk of long COVID and its symptoms present very differently across diverse populations and suggests that further investigation is needed to accurately define the disease and improve diagnosis and treatment.
The study, published April 7 in Nature Communications, analyzed electronic health records as part of the National Institutes of Health’s Researching COVID to Enhance Recovery (RECOVER) Initiative to better understand the persistence of symptoms after SARS-CoV-2 infection, also known as long COVID, among broad, diverse populations.
Led by Dr. Rainu Kaushal, chair of the Department of Population Health Sciences at Weill Cornell Medicine and physician-in-chief of population health sciences at New York-Presbyterian Hospital/Weill Cornell Medical Center, the research provides an overview of potential symptoms after acute COVID-19 and how the risk of these conditions may vary among different populations in the United States.
“Long COVID is a new disease that is very complicated and quite difficult to characterize,” said Dr. Chengxi Zang, an instructor in population health sciences at Weill Cornell Medicine and lead author on the paper. “It affects multiple organs and presents a severe burden to society, making it urgent that we define this disease and determine how well that definition applies among different populations. This paper provides the basis for furthering research on long COVID.”
The team studied electronic health records from two clinical research networks that are part of the National Patient-Centered Clinical Research Network (PCORnet). One dataset, from the INSIGHT Clinical Research Network—which Dr. Kaushal leads—included data from 11 million New York-based patients, while the other came from the OneFlorida+ network, which included 16.8 million patients from Florida, Georgia and Alabama.
The team identified a broad list of diagnoses that occurred more frequently in patients who had recently had COVID compared with non-infected individuals. The researchers also found more types of symptoms and higher risk of long COVID in New York City than Florida. Specific conditions found across the New York City and Florida populations included dementia, hair loss, sores in the stomach and small intestine, blood clots in the lung, chest pain, abnormal heartbeat and fatigue.
“Our approach, which uses machine learning with electronic health records, provides a data-driven way to define long COVID and determine how generalizable our definition of the disease is,” Dr. Zang said. Comparing records across diverse populations in regions that experienced the COVID-19 pandemic differently highlighted how variable long COVID is for patients and emphasized the need for further investigation to improve the diagnosis and treatment of the disease.
Some of the differences between the results from the two populations might be explained by the fact that New York City had a more diverse patient population, endured one of the first waves of the pandemic and faced the lack of personal protective equipment such as masks, compared with Florida, Dr. Zang said.
The new study is related to previous work by Dr. Kaushal, who is also senior associate dean for clinical research and the Nanette Laitman Distinguished Professor of Population Health Sciences at Weill Cornell Medicine, and colleagues, that categorized different subtypes of long COVID.
“In this new research, we examined a broad list of potential long COVID conditions one by one,” said Dr. Fei Wang, associate professor of population health sciences and co-senior author of the study. “These findings can help us better recognize the broad involvement of multiple organ systems in long COVID, and design appropriate plans for patient management and treatment development.”

Leave a Reply