by Hebrew SeniorLife Hinda and Arthur Marcus Institute for Aging Research
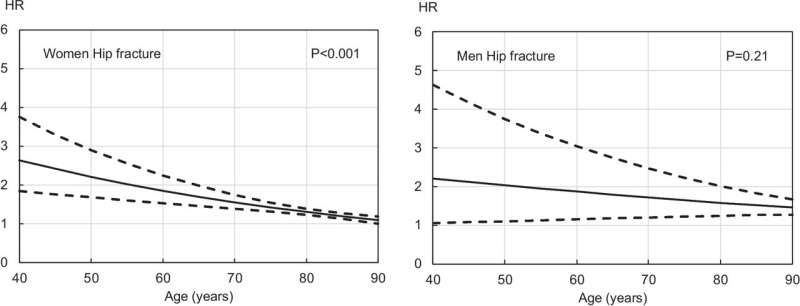
association with subsequent risk of a hip fracture in women (left panel) and men (right panel). Hazard ratios (HR), adjusted for duration of follow-up, and 95% confidence interval are shown. P values are for the interaction term with age at baseline. Credit: Osteoporosis International (2024). DOI: 10.1007/s00198-023-07012-1
A recent study titled “A meta-analysis of previous falls and subsequent fracture risk in cohort studies” found links between self-reported falls and increased fracture risk and also that prior falls increased the risk for fracture slightly more in men than women.
Published in Osteoporosis International, this international meta-analysis of data pooled from 46 prospective cohorts comprising over 900,000 individuals also recommended that previous falls are a factor that should be included in patients’ histories used by fracture risk assessment tools like the FRAX (Fracture Risk Assessment) Tool to calculate a person’s likelihood of getting a fracture over the next decade. FRAX is the most commonly used assessment to predict fracture risk.
“FRAX was developed using longitudinal data from studies around the world. Although previous falls have long been recognized as a significant risk factor for fractures, until now, they have not been factored into the FRAX algorithm,” said Douglas P. Kiel, M.D., MPH, director of the Musculoskeletal Research Center and senior scientist at the Hinda and Arthur Marcus Institute for Aging Research at Hebrew SeniorLife, a nonprofit, Harvard Medical School affiliated institution.
“In this newly updated FRAX dataset, previous falls were included as a risk factor and were found to increase the risk for fracture. These findings underscore that falls are an important contributor to fracture in both men and women, but interestingly, slightly more in men.”
Key findings of the meta-analysis include:
Increased Fracture Risk: Individuals with a history of falls within the past year were found to have a significantly higher risk of any clinical fracture, osteoporotic fracture, major osteoporotic fracture, and hip fracture. One or more previous falls were significantly associated with an increased risk of death among women and men.
Sex Disparities: The association between previous falls and fracture risk was observed to vary by sex, with men exhibiting higher predictive values compared to women.
Independent Risk Factor: The increased fracture risk linked to previous falls was largely independent of bone mineral density, emphasizing the standalone significance of falls as a risk factor. A previous fall in the past year confers a significantly increased risk of any clinical fracture, osteoporotic fracture, and hip fracture, with the increase in risk varying between 36% and 59% depending on the fracture outcome and sex.
“These findings underscore the importance of incorporating previous falls into the FRAX algorithm,” Dr. Kiel added. Integrating this information into tools like FRAX can enhance their predictive accuracy and ultimately help health care providers to more accurately predict fracture risk and tailor preventive strategies accordingly to improve patient outcomes.
More information: Liesbeth Vandenput et al, A meta-analysis of previous falls and subsequent fracture risk in cohort studies, Osteoporosis International (2024). DOI: 10.1007/s00198-023-07012-1
Provided by Hebrew SeniorLife Hinda and Arthur Marcus Institute for Aging Research

Leave a Reply