by University of California, San Francisco
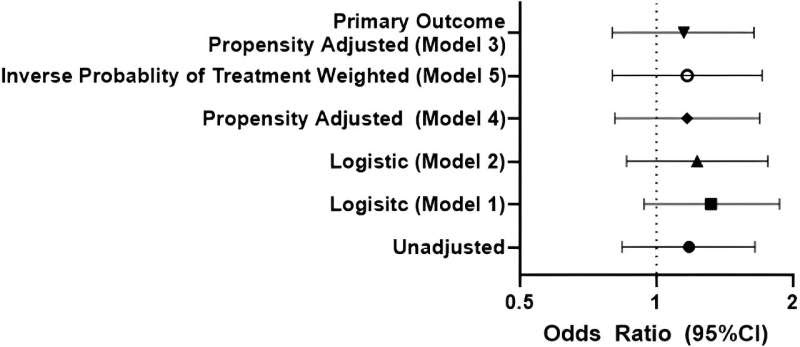
In all models, treatment with oral nirmatrelvir was not associated with lower odds of patient reported Long COVID symptoms with confidence intervals that cross 1, which suggests that treatment is not beneficial in reducing the risk of Long COVID. Model 3, the prespecified primary result, includes age, sex, and time since SARS-CoV-2 infection, and the restricted cubic spline of the propensity score. Model 1 includes age, sex, and time since SARS-CoV-2 infection. Model 2 includes age, sex, time since SARS-CoV-2 infection, race/ethnicity, past medical history and substance use. Model 4 is the propensity-adjusted version of Model 2. Finally, Model 5 incorporates inverse probability of treatment weighting and age, sex, and time since SARS-CoV-2 infection. Results were similar in additional sensitivity analyses. CI, confidence interval. Credit: Journal of Medical Virology (2024). DOI: 10.1002/jmv.29333
A team of researchers from UC San Francisco has found that Paxlovid (Nirmatrelvir-ritonavir) did not reduce the risk of developing long COVID for vaccinated, non-hospitalized individuals during their first COVID-19 infection. They also found a higher proportion of individuals with acute symptoms rebound and test-positivity than previously reported.
The study appears in the Journal of Medical Virology.
Paxlovid treatment for acute COVID-19 has been shown to be effective for high-risk unvaccinated individuals. But the effect of the treatment on long COVID risk, including whether it protects vaccinated people from getting long COVID, has been less clear.
The research team selected a group of vaccinated people from the UCSF COVID-19 Citizen Science study who had reported their first positive test for COVID-19 between March and August of 2022 and who were not hospitalized.
Some of these participants reported taking oral Paxlovid treatment during the acute phase of their COVID-19 infection, while others did not. In December of 2022, they were invited to answer a follow-up survey with questions about long COVID, COVID rebound symptoms, and how long they continued to test positive.
Researchers found the two groups were similar. About 16% of those treated with Paxlovid had long COVID symptoms compared to 14% of those who were not treated with the medication. Commonly reported symptoms included fatigue, shortness of breath, confusion, headache, and altered taste and smell.
Those who took Paxlovid and then went on to develop long COVID reported as many long COVID symptoms as those who were not treated with Paxlovid. A small percentage of people developed severe long-term COVID, and those who had received Paxlovid were just as likely to have severe Long-term COVID symptoms as those who did not.
Among individuals who experienced symptomatic improvement during Paxlovid treatment, 21% reported rebound symptoms. And among those with rebound symptoms, 10.8% reported one or more Long COVID symptoms compared to 8.3% without rebound symptoms. For participants who repeated antigen testing after testing negative and completing treatment, 25.7% reported rebound test positivity. In total, 26.1% reported rebound symptoms or test positivity.
“We found a higher proportion with clinical rebound than previously reported but did not identify an effect of post-treatment rebound on long COVID symptoms,” said study first author Matthew Durstenfeld, MD, MAS, a cardiologist and UCSF assistant professor of Medicine.
“Our finding that Paxlovid treatment during acute infection is not associated with lower odds of long COVID surprised us, but it is consistent with two other rigorously conducted studies finding no difference in post-COVID conditions between 4 and 6 months after infection.”
The authors note that the study may have been impacted by limitations arising from its observational nature with researchers relying on patient self-reporting of treatment and Long COVID symptoms.
More information: Matthew Durstenfeld et al, Association of Nirmatrelvir for Acute SARS-CoV-2 Infection with Subsequent Long COVID Symptoms in an Observational Cohort Study, Journal of Medical Virology (2024). DOI: 10.1002/jmv.29333
Provided by University of California, San Francisco

Leave a Reply