JULY 24, 2024
by University of Geneva
Credit: Unsplash/CC0 Public Domain
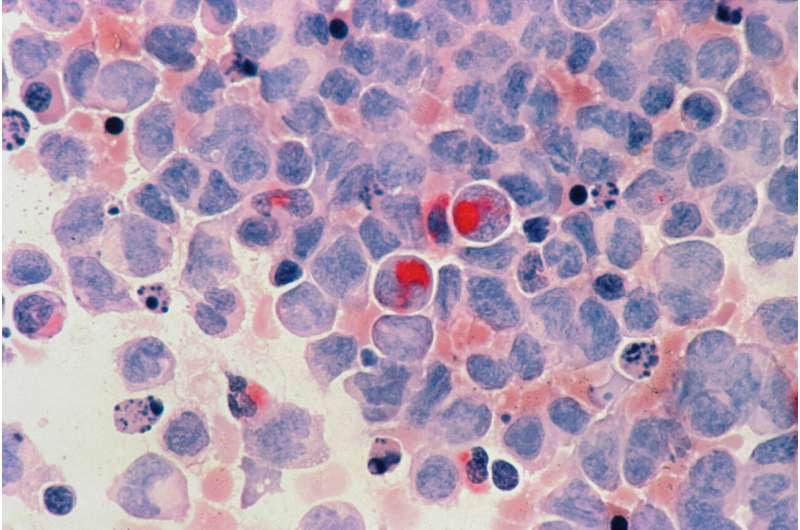
Acute myeloid leukemia (AML) is the most common blood and bone marrow cancer in adults. Caused by an increase in immature cells that rapidly destroy and replace healthy blood cells (red and white blood cells and platelets), AML is lethal in half of those affected under the age of 60, and in 85% of those over that age.
This unfavorable prognosis may be due to the presence of so-called dormant or quiescent leukemic stem cells (LSCs), which evade chemotherapy. Often invisible, these cells can wake up and reactivate the disease after an apparently successful course of treatment. Developing therapies that target these cells is therefore a major research challenge. However, the mechanisms controlling them are poorly understood.
By identifying genetic and metabolic characteristics specific to LSCs, a team from the University of Geneva (UNIGE), University Hospital of Geneva (HUG), and Inserm is providing new insights, as well as ways of combating the disease. These results, published in Science Translational Medicine, pave the way for a new therapeutic target and its clinical application.
“Using advanced bioinformatics techniques and in collaboration with the team of Dr. Petros Tsantoulis from the Department of Oncology and Precision Oncology at the HUG, we first established that these quiescent cells contain a unique genetic signature consisting of 35 genes. When we used this signature in large clinical databases of patients with AML, we were able to show that this signature was strongly linked to the prognosis of the disease,” explains Jérôme Tamburini, associate professor in the Department of Medicine and the Centre for Translational Research in Onco-hematology (CRTOH) in the UNIGE Faculty of Medicine and at the Swiss Cancer Center Léman (SCCL), staff physician in the Division of Oncology at HUG, who led this research.
Blocking a specific nutrient
The study also highlights a metabolic difference between dormant and active leukemic stem cells. In general, to survive, cells trigger chemical reactions that enable them to break down nutrients and thus produce energy.
This also involves autophagy, a process that allows cells to recycle cellular components to generate new ones and to provide energy in case of a lack of external nutrients. Scientists have discovered that dormant leukemic stem cells depend on ferritinophagy, a specific form of autophagy targeting ferritin, the main iron storage molecule.
“This process is mediated by a protein called NCOA4. It controls the availability of iron in cells. By inhibiting it, either genetically or chemically, we observed that leukemia cells, especially dormant stem cells, are more likely to die, whereas healthy blood stem cells remain intact,” says Inserm researcher Clément Larrue, a former post-doctoral researcher in Jérôme Tamburini’s group, currently a post-doctoral researcher at the Toulouse Cancer Research Center, and first author of the study.
Towards clinical trials
Experiments conducted with mouse models have confirmed that blocking the NCOA4 protein reduces tumor growth, viability and self-renewal of leukemic stem cells. Targeting ferritinophagy through this inhibition pathway could therefore be a promising therapeutic strategy. The compound used to block NCOA4 is in the early stages of development for future clinical trials, under the direction of one of the study’s co-authors, Jun Xu, a professor at Sun Yat-Sen University in China.
The next step for the UNIGE team will be to explore further the mechanisms of ferritinophagy and its association with mitophagy, another key mechanism in the regulation of LSCs. This new stage of research is supported by the Swiss Cancer League.
More information: clement larrue et al, Targeting ferritinophagy impairs quiescent cancer stem cells in acute myeloid leukemia in vitro and in vivo models, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adk1731. www.science.org/doi/10.1126/scitranslmed.adk1731
Journal information: Science Translational Medicine
Provided by University of Geneva

Leave a Reply