by The Mount Sinai Hospital
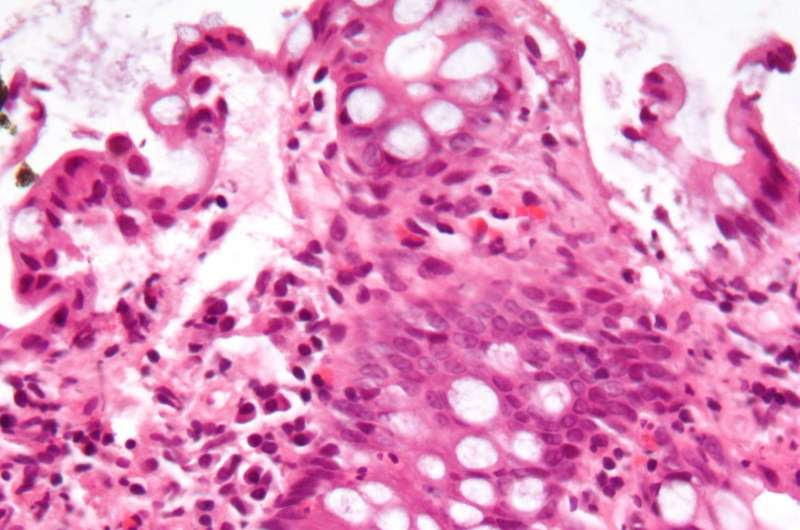
Micrograph showing inflammation of the large bowel in a case of inflammatory bowel disease. Colonic biopsy. Credit: Wikipedia/CC BY-SA 3.0
Mount Sinai researchers have published one of the first studies to demonstrate the importance of reactive oxygen species in maintaining stem cell function and preventing inflammation during wound repair, which could provide greater insights into the prevention and treatment of inflammatory bowel diseases (IBD), according to findings published in the journal Gut on October 3.
Reactive oxygen species are highly reactive chemicals formed from oxygen. They serve as prime signals of cellular dysfunction that contribute to diseases. Secretion of reactive oxygen species in the intestine is necessary for maintaining stem cell function and important for wound repair; however, it can cause inflammatory effects as well. The Mount Sinai team found the key transcription factors driving abnormal stem cell changes, suggesting a significant role of reactive oxygen species in maintaining healthy intestines.
“While it’s clear that regulation of oxygen and reactive oxygen species plays a critical role in chronic diseases generally, and IBD in particular, this study provides a major advance in defining the key role of oxygen species in maintaining a healthy epithelial barrier for IBD,” said senior author Judy H. Cho, MD, Dean for Translational Genetics and Ward-Coleman Chair in Translational Genetics, and Vice Chair of Pathology, Molecular and Cell-Based Medicine at the Icahn School of Medicine at Mount Sinai.
The research team studied the role of reactive oxygen species and NOX1, the protein used to produce these chemicals, by examining single-cell gene expression in vitro and in vivo in mice models, as well as ex vivo in the form of human intestinal biopsies obtained following routine colonoscopies. They measured the amount of reactive oxygen species and analyzed the gene expression profile of intestine barrier cells from mice and human patients with a subtype of IBD known as ulcerative colitis. Intestine barrier cells cover the intestine surface and help to digest food, absorb nutrients, and prevent the invasion of gut bacteria. The Mount Sinai researchers compared gene expression data in both inflamed and uninflamed colon tissues.
The researchers found that a combination of NOX1, loss of function—which results in decreased reactive oxygen species, plus the presence of a substance known as TNF that causes inflammation leads to an abnormal increase of microfold cells. Microfold cells, also known as M cells, are crucial to regulating gut immune response. The research team found this abnormal increase in M cells, as a result of loss of reactive oxygen species, in stem cells in both the human and mice models. This increase in epithelial M cells drives increased recruitment of immune cells in mice. By treating intestine cells with reactive oxygen species, they were able to reverse the initial defect caused by losing reactive oxygen species during inflammation.
“Reactive oxygen specifies released by stem cells are critical in maintaining a heathy gut via maintaining proper balance of intestine barrier cell types,” said lead author Nai-Yun Hsu, Ph.D., Associate Scientist in the Judy Cho Laboratory. The researchers encourage further studies, which they said could include direct reactive oxygen species-stem cell modulation therapy to IBD patients in future treatments.
The University of Oxford in Oxford, United Kingdom, contributed to the research.

Leave a Reply