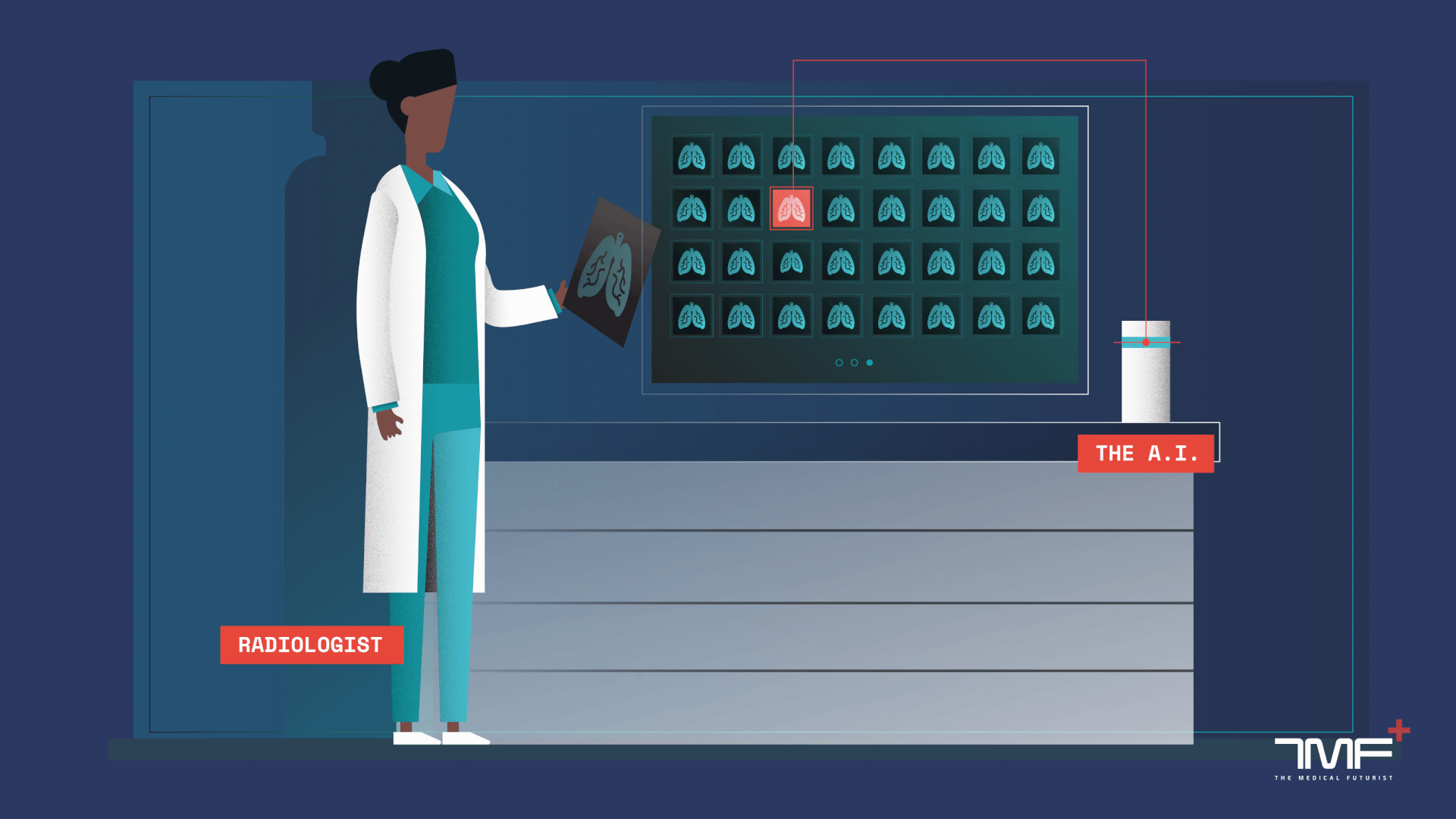
As artificial intelligence tools have been invading more or less every area of healthcare, we made a list to keep track of the top A.I. algorithms aiming for better diagnostics, more sophisticated patient care or further sighted predictions of diseases.
The Medical Futurist
Does A.I. beat doctors?
Only if you have lived under a rock for the last couple of years could you not have heard about artificial intelligence. Some might have even come across the spread and potential of A.I. in healthcare. Not only smart algorithms themselves but also the hype around A.I. has grown immensely, thus every time a new study about deep learning or machine learning in diagnostics, in medical imaging or any other medical field gets published, newsreaders can be sure that some titles will say that “A.I. has again beaten doctors in field X”.
The narrative is so distorted towards extreme visions that artificial intelligence is either presented as the ultimate evil destroying mankind – both Elon Musk and Stephen Hawking warned about that – or the only source of the future prosperity of humanity. For mitigating the damaging effects of hype and to see a clearer picture in the “battle” between A.I. and mankind, the Institute of Electrical and Electronics Engineers (IEEE) created an excellent visualization tool to see whether smart algorithms or humans are better in providing healthcare solutions.
By enumerating the top A.I. tools that we discovered in healthcare so far, we also aim to add what we believe is already useful for the work of medical professionals.
Life is no training data set
Artificial intelligence has numerous limitations just as yet, so before we present our list, it’s worth going through them one by one. Already the term is misleading as A.I. implies a far more developed technology where it is standing at the moment. At best, current science – meaning various machine learning methods – is able to reach artificial narrow intelligence (ANI) in multiple fields, the first level of intelligence created by humans. It means what algorithms running on ever more powerful computers can currently do is recognizing patterns and gleaning topics from blocks of text or deriving the meaning of whole documents from a few sentences. Yet, we are nowhere close to artificial general intelligence (AGI), the second level of intelligence when a machine is capable of abstracting concepts from limited experience and transferring knowledge between domains. The third and most fearful domain, superintelligence, when A.I. evolves into a stand-alone consciousness, is nowhere close.
Yet, ANI and its two main streams, natural language processing, and computer vision, are developing at an incredible speed. The latter is crucial for diagnostics in healthcare as it is based on pattern recognition. Countless algorithms are currently trained to categorize various patterns seen in medical images and thus help doctors diagnose conditions.
The limitations of such studies are present in at least three areas. At first, used medical evidence tends to originate from highly developed regions containing their specificity or the framework for conceptualizing the algorithm itself incorporates the subjective assumptions of the working team. Secondly, the forecasting and predictive abilities of smart algorithms are anchored in previous cases – however, they might be useless in new cases of drug side-effects or treatment resistance.
Finally, the majority of the already conducted A.I. research has been done on training data sets collected from various medical facilities and after the algorithm analyses the images, doctors are provided with the same dataset – usually without reproducing the clinical conditions.
That does not decrease the theoretical value of the study – but its practical implementation. Life is no training data set. Thousands of patients come and go to a hospital with thousands of symptoms and describe similar or the same conditions very differently. Thus, the results of A.I. studies conducted on training data sets might not be representative of what would happen in real-life situations. Common interpretations often leave out these limitations focusing on presenting these studies as ultimate revelations.
Keeping all these constraints in mind, here are the top A.I. algorithms that we recently found in healthcare.
Artificial IntelligenceIllustration by Björn Oberg
1) The algorithm spotting DNA mutations in tumors
One of the reasons why it’s so incredibly difficult to treat cancer is that malignant tumors tend to mutate, grow, evolve and change. In the last years, scientists discovered that not only cancer itself transforms but so does its DNA. As sequencing costs significantly dropped, the genetic analysis of tumors became possible, and recently, human experts with the support of computational tools started to analyze the data to figure out what kinds of genetic changes, or mutations, occur.
For making such existing tools more precise, Personal Genome Diagnostics in Baltimore developed a new method involving machine learning that automates the tumor DNA diagnostic process and improves the accuracy of identifying mutations in cancerous tissues. Bearing that result in mind, the doctor can choose the specific targeted treatment for the patient.
2) Can A.I. score better in classifying heart images than humans?
Echocardiograms produce sound waves to paint the heart’s picture – from which cardiologists can identify whether the patient has any heart disease. It’s a standard test to check for problems with valves or chambers of our central organ, for congenital heart defect or whether shortness of breath or chest pain is in connection with the heart.
Rima Arnaut, an assistant professor and practicing cardiologist at UC San Francisco and her colleagues used deep learning to train an A.I. system that can classify echocardiograms according to the type of view shown. When both the A.I. and expert cardiologists were asked to sort the images, the algorithm achieved an accuracy of 92 percent. The humans got only 79 percent correct.
3) Heart attack predicting algorithm
Smart algorithms do not only outperform doctors when it comes to classifying but also in predicting outcomes based on various factors. Recently, researchers at the University of Nottingham in the UK created a system that scanned patients’ routine medical data and predicted which of them would have heart attacks or strokes within 10 years. When compared to the standard method of prediction based on well-established risk factors such as high blood pressure, cholesterol, age, smoking, and diabetes, the A.I. system correctly predicted the fates of 355 more patients.
That’s a significant achievement for an A.I. system, especially when keeping in mind how difficult it is to predict heart attacks and strokes. The researchers believe that the algorithm might be in clinical use within the next five years.
4) More precise skin cancer diagnoses with A.I.
According to statistics from the WHO, currently, between 2 and 3 million non-melanoma skin cancers and 132,000 melanoma skin cancers occur each year globally. Digital health technologies, such as smartphone apps like SkinVision, telemedical services as well as A.I. are at the frontlines of fighting the widely prevalent disease.
Although several research groups developed smart algorithms for diagnosing skin cancer already, the one created at Stanford University is likely the most robust system so far. It was trained on more than 1.28 million images and fine-tuned with a set of nearly 130,000 scans of skin lesions from more than 2000 diseases. That’s the most extensive dataset used for automated skin cancer classification as of yet.
5) A.I. systems for the ICU
Intensive care units are battlegrounds for human lives. As every moment counts, patients are monitored 24/7 with an army of devices. Constantly beeping bedside monitors show blood pressure, heart rate or any other vital signs of the patient, a machine takes care of the function of the lungs as best as possible, and another goes for the heart. However, these instruments are usually not connected, they are isolated units in the concert of ICU care.
The US-based company, Autonomous Healthcare, aims to change exactly that. They are working on some of the first A.I. systems for the ICU, an “algorithmic expert” constantly at the bedside of the patient connecting the dots and carefully calibrating treatment.
6) Computers detecting breast cancer risk
Breast cancer is the most commonly occurring cancer in women and the second most common cancer overall. In spite of global awareness raising and prevention efforts, there were over 2 million new cases in 2018. The WHO estimates that over 508 000 women died in 2011 due to breast cancer worldwide.
As in the case of many other cancer types, early detection could be live saver. However, women with dense breasts have a higher risk of undergoing mammogram screenings that miss signs of breast cancer. Researchers at the University of California, San Francisco found that commercial software for automatically classifying breast density and thus detecting breast cancer is just as accurate as human radiologists. Shortly, the algorithm could support doctors with cases when breast density would not allow clear diagnosis.
7) A.I. helps pathologists diagnose metastatic breast cancer
Algorithms could not only assist radiologists but also pathologists in their fight against breast cancer. The International Symposium on Biomedical Imaging (ISBI) held a grand challenge to evaluate computational systems for the automated detection of metastatic breast cancer. The winning study showed that combining the efforts of the human pathologist and the deep learning system’s predictions, the human error rate decreased by 85 percent when identifying metastatic breast cancer.
That’s an impressive result, especially bearing in mind that early diagnosis means saving lives when it comes to the lethal disease. Beyond the achievement, it is worth noting that the joint efforts of A.I. and human doctors indicated a significant improvement in diagnosing, their single results were not even close.
8) Smart algorithm predicting suicide risk
In the future, you might go to the hospital with a broken arm and leave the facility with a cast and a note with a compulsory psychiatry session due to flagged suicide risk. That’s what some scientists aim for with their A.I. system developed to catch depressive behavior early on and help reduce the emergence of severe mental illnesses.
The machine learning algorithm created at Vanderbilt University Medical Center in Nashville, uses hospital admissions data, including age, gender, zip code, medication, and diagnostic history, to predict the likelihood of any given individual taking their own life. In trials using data gathered from more than 5,000 patients who had been admitted to the hospital for either self-harm or suicide attempts, the algorithm was 84% accurate at predicting whether someone would attempt suicide the following week, and 80% accurate at predicting whether someone would attempt suicide within the following two years.
9) A.I. predicting death risk among inpatients
Researchers at Stanford University trained an A.I. system to increase the number of inpatients who receive end-of-life-care exactly when needed – meaning the smart algorithm is able to predict when very seriously ill patients are nearing the end of their lives.
The algorithm was trained to analyze diagnoses, prescriptions, demographics, and other factors within electronic health records during that 3 to 12 month period before a patient passed away. Once trained, the algorithm was able to flag still-living patients in a hospital’s system that might be appropriate candidates for palliative care. When Stanford Hospital’s palliative care team assessed 50 randomly chosen patients that the algorithm had flagged as being at very high risk, the team found that all of them were appropriate to be referred. Beyond being able to accurately predict, the program also left decision-making in the hands of the doctor entirely. That could be a future model for algorithms and physicians working together as a team.
There are many more excellent examples of smart algorithms in healthcare, and a lot more will come in the future. But the last one showed the essence of digital health: the best results are achieved by the cooperative work of artificial intelligence and human doctors.
That’s the future we aim for: the harmonious collaboration of digital technologies and people for the greater good of humanity.

Leave a Reply