JULY 24, 2024
by Ingrid Fadelli , Medical Xpress
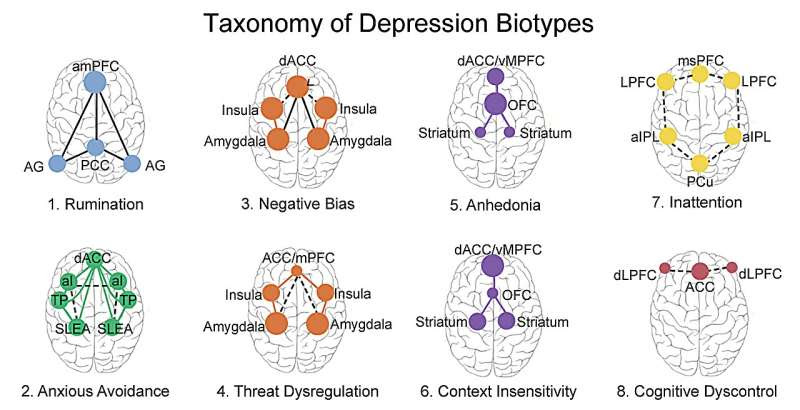
Overview of biotypes that underlie the heterogeneity of clinical depression and associated depression, and which can be assessed using functional magnetic resonance imaging to quantify the activity of brain regions and the functional connectivity between brain regions. Credit: Williams LM. Precision psychiatry: a neural circuit taxonomy for depression and anxiety. Lancet Psychiatry. 2016 May;3(5):472-80. doi: 10.1016/S2215-0366(15)00579-9. Epub 2016 Apr 14. PMID: 27150382; PMCID: PMC4922884.
Depression is one of the most common mental health disorders worldwide, estimated to affect about one in eight people worldwide. Once individuals experiencing symptoms of depression approach a psychiatrist or psychotherapist, they are often rapidly diagnosed, yet identifying a treatment strategy that works for them is not always as simple.
In many cases, individuals who are diagnosed with depression undergo a tiring and potentially taxing process of trial-and-error, which consists of trying a treatment, waiting to determine if it is helping and trying another if it proves ineffective. This process can sometimes take years, with approximately 30% of depressed patients becoming treatment resistant.
In recent years, some psychiatry researchers and neuroscientists have thus been trying to identify types of depression that respond differently to specific treatments. These efforts led to the identification of a particular ‘biotype’, which is marked by a dysfunction in the brain’s cognitive control circuit, a lower quality of life, increased disability and, in many cases, a resistance to available treatment options.
Researchers at Stanford University School of Medicine, VA Palo Alto Health Care System and other institutions across the United States recently set out to assess how patients with this biotype of depression responded to transcranial magnetic stimulation (TMS), a procedure that entails the stimulation of brain nerve cells using magnetic fields.
Their findings, published in Nature Mental Health, suggests that TMS could help to treat patients exhibiting this specific depression biotype, which could open interesting possibilities for precision psychiatry.
“The primary inspiration for our study was to help personalize treatment approaches by identifying more precise subtypes of depression, which we call ‘biotypes,'” Leanne Williams, co-senior author of the paper, told Medical Xpress. “Our research focuses on the concept that clinical depression is composed of various biotypes, each responding differently to specific treatments.”
In their previous research, Williams and her collaborators identified a cognitive biotype of depression that responds poorly to conventional antidepressant medications. The primary objective of their recent study was to determine whether patients with this biotype could benefit from TMS, both in terms of their cognitive control and behavior.
“Currently, TMS is reserved for treatment resistant patients whose depression hasn’t responded to multiple antidepressant trials,” Williams explained. “However, we lack a test to identify early on which patients might benefit from TMS. A test based on the cognitive control biotype could allow patients to bypass the lengthy trial-and-error process and proceed directly to incorporating TMS into their treatment.”
This recent study was carried out in collaboration with the National Veterans Administration (VA), which is running a TMS clinical program. This program allowed the researchers to study the effects of TMS on mental health disorders within a real-world setting, as opposed to laboratory environments that impose strict experimental criteria.
“I was the principal investigator (PI) for this study, while co-senior author Dr. Michelle Madore, the director of the National TMS clinical program based at the Palo Alto VA, facilitated the study across four VA sites,” Williams said.
“These sites and the co-PIs for each site include Palo Alto VA (with Stanford University as the academic affiliate), White River Junction VA (with Dartmouth University, Dr. Paul Holtzheimer), Providence VA (with Brown University, Dr. Noah Philip), and Minneapolis VA (with the University of Minnesota, Dr. Kelvin Lim).”
As part of the VA’s clinical program, veteran patients with treatment-resistant depression received TMS. Williams and their colleagues studied the brains and cognitive abilities of these patients using functional magnetic resonance imaging (fMRI) and cognitive tests, respectively.
The researchers’ study involved a total of 43 veterans, who were assessed before receiving TMS, as well as after the first and after several treatment sessions. Individual veteran patients who were taking part in the TMS clinical trial were referred to one of the four sites involved in the study to undergo fMRI and complete cognitive tests.
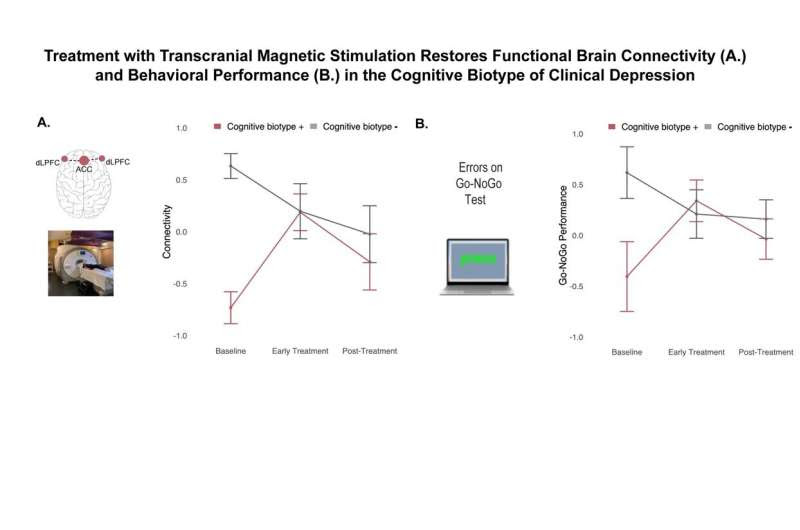
TMS produced an early improvement in cognitive control circuit connectivity that was specific to Veterans with depression who had a cognitive biotype (cognitive biotype +) at the pre-TMS baseline (A.). TMS also produced an early restoration of cognitive performance in cognitive biotype + Veterans with depression (B.). This early improvement for brain connectivity and performance persisted post-treatment with TMS. Credit: Tozzi, L., Bertrand, C., Hack, L.M. et al. A cognitive neural circuit biotype of depression showing functional and behavioral improvement after transcranial magnetic stimulation in the B-SMART-fMRI trial. Nat. Mental Health (2024). DOI: 10.1038/s44220-024-00271-9
“We used fMRI scans to obtain a baseline biotype of their brain, quantified by our Stanford Et Cere image processing method,” Williams explained.
“We conducted this first scan before they started TMS. Early in the treatment, after five TMS sessions, we performed a second fMRI scan to assess early changes in brain function. A third and final fMRI scan was conducted post-treatment, after the completion of all TMS sessions.”
The patients’ cognitive performance was evaluated using a computer-based test, known as the Go-NoGo test. These tests were designed to assess the ability of patients to process information and plan actions accordingly.
Using the baseline biotype information collected in their previous studies, Williams and her colleagues were able to categorize the patients who took part in their study into two groups: those with the biotype present (cognitive biotype +) and those without it (cognitive biotype -).
They found that approximately half of the participants exhibited signs of the cognitive biotype, which was reflected in a reduced functional connectivity in their brain’s cognitive control circuit and poorer performance on the Go-NoGo test.
“Through statistical modeling, we demonstrated that TMS significantly improved both functional brain connectivity and cognitive performance specifically for the cognitive biotype + group,” Williams said.
“This remarkable improvement was observed after just five sessions of TMS. By the final post-treatment assessment, the improvements were substantial enough that there was no longer a significant difference between cognitive biotype + and cognitive biotype—patients.”
The findings gathered by Williams and her colleagues suggest that patients with the cognitive and treatment-resistant biotype of depression could benefit from TMS. Specifically, TMS was found to both improve cognitive function and foster more adaptive behaviors in these patients.
“Cognitive impairments in depression are major contributors to years lost due to disability and increased suicide risk,” Williams said.
“These lost years are why clinical depression is currently the leading cause of disability worldwide, surpassing any other medical illness. Our findings suggest that using biotype tests could help match patients with the most effective treatment for them much sooner than the current trial-and-error approach allows.”
The results of this recent study could have important clinical implications, as it could inform the development of diagnostic tests and interventions aimed at identifying and treating the cognitive biotype of depression. For instance, patients with this biotype could be offered TMS as a treatment option before they develop a resistance to treatments, which could significantly improve their quality of life.
“By reducing the disability associated with depression through a precise biotyping strategy, we also expect to decrease the economic impact of clinical depression,” Williams said.
“Currently, clinical depression is linked with the highest direct and indirect costs among all medical conditions for both individuals and society, including negative effects on time management and productivity loss.
“Our findings support the precision mental health priorities of both the National Institute of Mental Health and the VA. The Scott Hannon Initiative for Precision Mental Health (SHIP-MH), signed into law in October 2020, directs the VA to advance precision strategies, including implementing functional magnetic resonance imaging to identify more precise subtypes and develop more personalized treatments to improve lives.”
Williams and her colleagues hope to continue contributing to the advent of precision psychiatry. As part of their future work, they plan to run prospective clinical trials aimed at identifying the most effective treatments for each biotype of depression and then promptly offer targeted treatments to individual patients.
“We are expanding our fMRI and behavioral research to include more participants and collaborating sites,” Williams added.
“Our goal is to scale up our research by testing more treatments across all six biotypes and using AI to refine existing biotypes and discover new ones. This expansion will link brain imaging biotypes with clinical and digital measures, potentially enabling remote monitoring that can be interpreted in terms of underlying brain function.”
The Stanford Et Cere imaging technology required to identify the biotypes of depression is already being deployed both at Stanford and at other sites in the US. The researchers are working to make this technology as accessible as possible, in the hope that it will reach a growing number of clinicians and patients worldwide.
More information: Leonardo Tozzi et al, A cognitive neural circuit biotype of depression showing functional and behavioral improvement after transcranial magnetic stimulation in the B-SMART-fMRI trial, Nature Mental Health (2024). DOI: 10.1038/s44220-024-00271-9.
Journal information: Nature Mental Health , The Lancet Psychiatry
© 2024 Science X Network

Leave a Reply