September 2, 2024
by Walter and Eliza Hall Institute of Medical Research
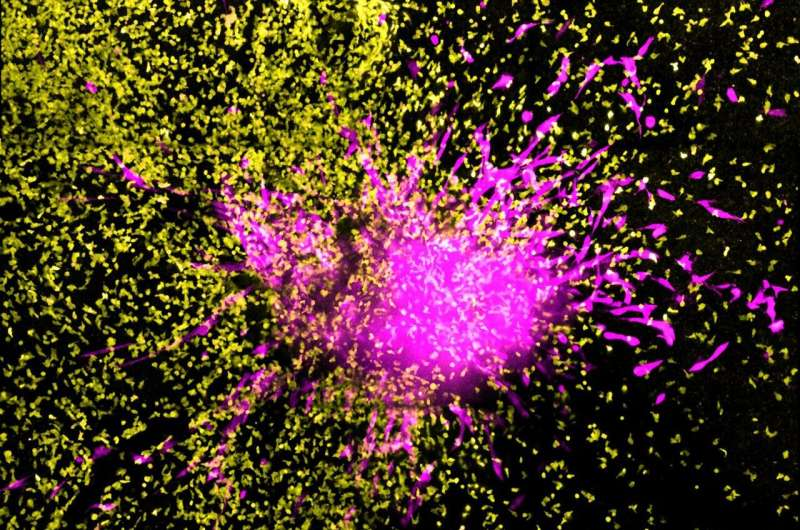
Chimeric antigen receptor (CAR) T cells, genetically engineered leukocytes (white blood cells), in their fight against glioblastoma, a deadly type of glioma. Credit: Journal for ImmunoTherapy of Cancer (2024). DOI: 10.1136/jitc-2024-009486
Researchers at WEHI have identified a promising new two-in-one treatment that not only targets and destroys an aggressive form of brain cancer, but also helps the immune system develop a lasting defense against it.
This dual-action approach uses a specific immunotherapy known as CAR T cell therapy to treat gliomas, an incurable brain cancer with few treatment options.
The pre-clinical findings have revealed the therapy’s ability to eliminate glioma cells and its potential to strengthen the immune system to prevent future tumor growth—two significant advances that could revolutionize the way these lethal cancers are treated in the future.
The paper is published in the Journal for ImmunoTherapy of Cancer.
Overcoming barriers to save lives
In Australia, one person is diagnosed with brain cancer every 5 hours. There currently is no cure and current therapies for severe brain cancers like gliomas are largely ineffective, leaving patients with few options.
CAR T cell therapy is an innovative new approach that involves isolating a patient’s immune cells, engineering them to become “super killer cells” and then re-infusing them into the patient to fight their cancer.
While CAR T cell therapy has shown promise for brain cancer treatment, finding the right proteins to target brain cancer cells has been a major hurdle.
The WEHI-led study has revealed a protein called EphA3, found on the surface of high-grade glioma cells, could be a key target for CAR T cell therapy.
Lead researcher and laboratory head at WEHI, Professor Misty Jenkins AO, says the potential impact of this discovery is profound on many levels.
“This new way to treat gliomas could offer a potential lifeline for patients,” Prof Jenkins, also head of the immunotherapy program at The Brain Cancer Center, said.
“Our research has shown that EphA3-targeted CAR T cells can effectively seek out and eliminate glioma cells, both in lab tests and animal models. This therapy not only targeted and killed the cancer cells, but also triggered a long-lasting immune response, preventing future tumor growth.
“We never expected a two-in-one breakthrough that could offer such life-saving possibilities. This is a significant development because gliomas are incredibly challenging to treat, and current options are limited.
“Most importantly, this could mean longer survival times for patients and improved quality of life, giving hope to those affected by these aggressive cancers.”
Future of cancer medicine
Prof Jenkins said CAR T cell therapy was opening up new pathways for brain cancer treatment.
“CAR T cell therapy is clever because it uses a patient’s own immune cells and engineers them to recognize and kill the tumor, with no long-term side effects,” she said.
“The tricky nature of brain cancer means that traditional methods don’t work—chemotherapy is ineffective, and radiation kills cancerous and healthy brain tissue.
“This recent discovery is further evidence that immunotherapy is a powerful force that can help overcome many cancer challenges that were previously considered insurmountable.”
Powerful new tools for cancer treatment
The project team is hopeful that future clinical trials for EphA3-targeted CAR T cell therapy could lead to the development of a treatment that not only kills and halts cancer growth, but also provides lasting immunity.
As the research advances, there is hope that partnerships with biotech companies and investors will help bring this innovative therapy to patients as quickly as possible.
“The possibility of providing patients with a long-lasting immune response against their cancer is a game-changer, offering a significantly better outlook for patients and their families,” Prof Jenkins said.
“The potential to revolutionize brain cancer treatment—like what has been achieved for other cancers—makes this a truly exciting time in the field of cancer research.
“As we stand on the brink of transforming brain cancer treatment, we are not just aiming for better outcomes—we’re striving for a future where the words ‘brain cancer’ no longer carry the same fear. The journey ahead promises breakthroughs that will redefine hope for patients around the world.”
More information: Leesa Lertsumitkul et al, EphA3-targeted chimeric antigen receptor T cells are effective in glioma and generate curative memory T cell responses, Journal for ImmunoTherapy of Cancer (2024). DOI: 10.1136/jitc-2024-009486
Journal information: Journal for ImmunoTherapy of Cancer
Provided by Walter and Eliza Hall Institute of Medical Research

Leave a Reply