by Brigham and Women’s Hospital
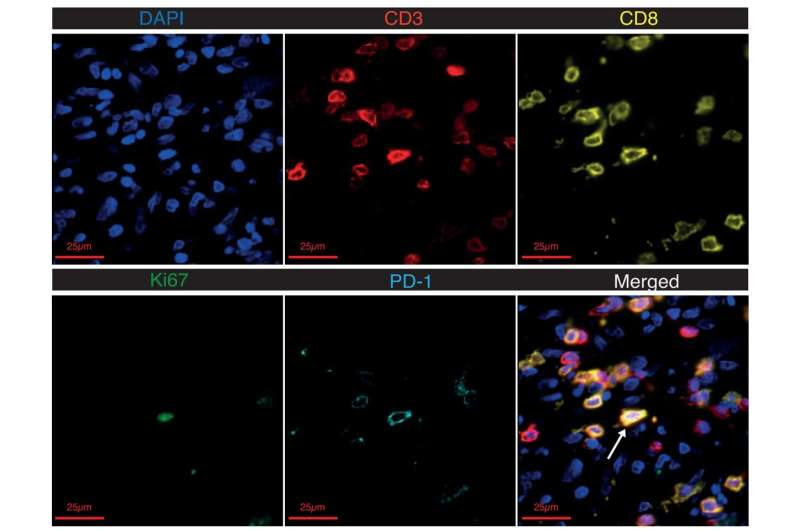
Multiplexed immunofluorescence of synovial tissue. Multiplexed immunofluorescence images showing an example of a Ki67+PD-1+ synovial CD8 T cell (white arrow). CD3 staining is shown in red, CD8 in yellow, nuclear stain DAPI in blue, Ki67 in green and PD-1 in cyan. Credit: Science Immunology (2023). DOI: 10.1126/sciimmunol.add1591
Immune checkpoint inhibitor (ICI) therapies used to treat cancer come with the risk of adverse autoimmune responses, including arthritis that can persist for years and require joint replacement surgery. Little is known about the specific cells responsible for these events.
Researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham health care system, and collaborators led a study to investigate these immune adverse events and identified a specific type of CD8 T cell that characterizes inflammatory arthritis induced by ICI therapies. Their findings are published in the journal Science Immunology.
Researchers studied T cells from a patient with severe ICI-arthritis who required bilateral knee replacements. In addition to these two joint tissue samples, they studied the fluid that accumulates within joints from an additional 23 patients with this condition and compared these samples to samples from patients with two common autoimmune conditions, rheumatoid arthritis or psoriatic arthritis.
By comparing protein and gene expression levels across diseases, they were able to characterize unique immunological features of the CD8 T cells in ICI-arthritis. They further identified that a specific set of cytokines, type I interferons, can promote the CD8 T cell activation seen in ICI-arthritis.
Patients whose cancer was treated with ICI had high levels of this CD8 T cell type, and additional analysis revealed that the cells traveled between the joints and blood. Further, the T cells persisted in the bloodstream, providing one explanation for why ICI-arthritis continues even after ICI therapy is discontinued. Limitations include a small cohort of patients who are taking various treatments. Further research is needed to characterize how the CD8 T cells contribute to joint inflammation.
“Our results suggest that ICI therapy gives rise to a unique population of CD8 T cells in patients who develop ICI-arthritis,” said co-corresponding author Deepak A. Rao, MD, Ph.D., of the Brigham’s Division of Rheumatology, Inflammation, Immunity. “The immune events we characterized differ dramatically from the typical responses we have seen in autoimmune diseases like rheumatoid arthritis and psoriatic arthritis.”

Leave a Reply