Written by Angela Haupt | Reviewed by Patricia Pinto-Garcia, MD, MPH
Published on October 13, 2023
Key takeaways:
Blood clots can happen anywhere in the body but are common in the legs. Clots can also break off and travel to the lungs.
Risk factors for blood clots include surgery, sitting for a long time, and taking hormonal birth control.
If you have a blood clot, you might experience symptoms such as leg swelling, sudden shortness of breath, sharp chest pain, back pain, and a rapid heart rate.
GoodRx Health
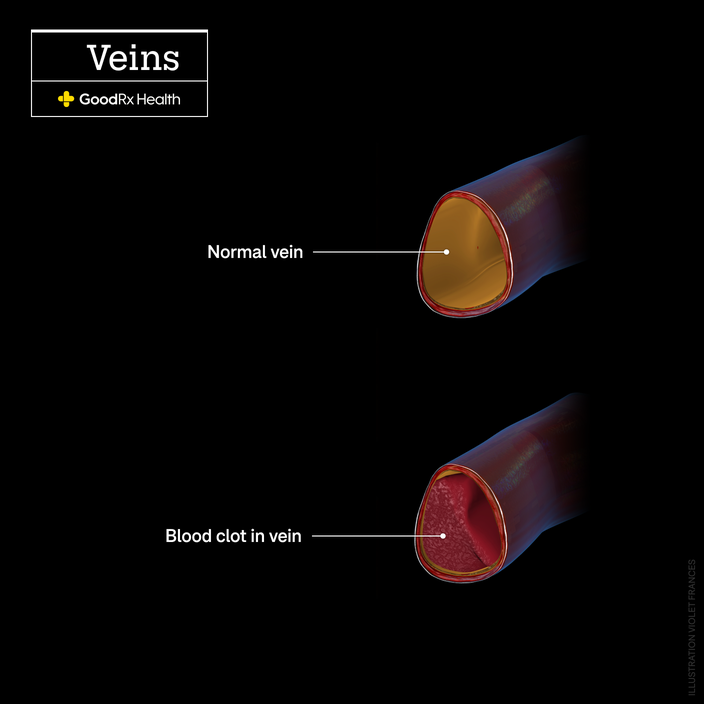
Blood naturally clots. It’s what prevents us from bleeding excessively. But sometimes, blood cells stick together when they shouldn’t, causing dangerous clots.
People of all ages and genders can develop blood clots anywhere in the body. Clots often form in the legs, which is called deep vein thrombosis (DVT). They can also break off and travel through the bloodstream and into the lungs, causing a pulmonary embolism (PE).
Some of the risk factors for blood clots include major surgery or illness, severe physical trauma, sitting too long, and using birth control that contains estrogen. Because blood clots can be fatal, it’s important to know the signs and symptoms. DVT, for example, can cause leg swelling and pain, as well as reddish or blue skin. Someone who has a PE might experience sudden shortness of breath, sharp chest pain, back pain, a rapid heart rate, and an unexplained cough.
Blood clots are typically treated with blood-thinning medications like Xarelto (rivaroxaban) and Eliquis (apixaban), which can break up existing clots and prevent new ones from forming or getting bigger.
Here, three people describe what it feels like to have a blood clot.
The blood clot that stole Christmas
A few weeks before Christmas 2021, Christine DiBugnara woke up with a burning sensation in her chest. Being an active person, she dismissed it as something exercise-related. Then, she had “really random jaw pain” — which she blamed on all the turkey jerky she had been eating. She also started experiencing frequent, terrible headaches.
As the weeks progressed, Christine’s pain moved into her back, and she went to the emergency room (ER). The doctors there assumed she had pulled a muscle and sent her home with steroids. “It was this terrible spasming pain in my rib area, like nothing I’d ever felt before,” says Christine, 46, who lives in Redondo Beach, California.
The steroids helped for the first couple days, but then her back pain worsened. “It was the worst pain of my life,” Christine recalls.
She tried to tough it out but, on Christmas Day, she went back to the emergency room. This time, she was diagnosed with bilateral pulmonary embolisms. She also experienced lung infarction, meaning some of her lung tissue died because of inadequate blood supply. At the time, Christine had been on hormonal birth control for more than 20 years, and her doctor told her that’s likely what led to her blood clots.
The ER doctors gave Christine blood thinners immediately, and she was discharged from the hospital after a day. When she got home, she was still dizzy and short of breath. The days that followed, she says, were a roller coaster.
“It was the worst feeling, going to bed at night thinking, ‘I’m not going to wake up,’” she says. Her entire torso, and especially her back, hurt. She ended up back in the hospital within a week because she was coughing up blood as her body adjusted to the blood thinners.
Christine’s recovery was tough. For months, she could only walk 5 minutes at a time. It took a year before she started to feel like parts of her old self were returning. In addition to taking blood thinners for 6 months, she went to physical therapy and talked about her “medical PTSD,” or post-traumatic stress disorder, with a therapist.
Her follow-up scans have revealed that there are no lingering blood clots. Though, she does have permanent lung scarring.
“I’m different now,” Christine says. “My body is not the same. It’ll never be the same. But I like to tell people that your new normal can still make you happy. You’re going to find that fire again in a totally different way.”
Scary-bad back pain
In 2022, Michelle Glogovac celebrated her 41st birthday with a happy, healthy day on the beach. Later that weekend, she woke up in the middle of the night with sharp back pain. It felt like a pinched nerve, she recalls, like the kind she had when she was pregnant years before.

Michelle, who’s now 42 and lives in San Jose, California, was still in a lot of pain the next morning. She was also unusually exhausted. That evening, when she and her husband were watching TV, her back pain got even worse.
“All of a sudden, I shot off the couch, I was in so much pain,” she says. “I got on my knees, and I saw stars — everything was going black.”
She tossed and turned all night, and emailed her doctor at 4AM saying she was in serious pain. Later that day, she decided to go to the ER.
Michelle’s blood tests indicated that she might have a blood clot, so the ER doctors gave her a CT scan. Her back pain was so severe that she could hardly lie down during the scan.
“I was in tears,” she says. She couldn’t get off the table by herself, so the technician helped her down, and she cried the entire way back to the exam room.
Within half an hour, a doctor informed Michelle that she had a pulmonary embolism. She was immediately given blood thinners and admitted to the hospital. During her stay, she had a thrombectomy, a surgical procedure to remove the blood clot and repair damaged blood vessels. After 5 days, she was discharged.
Once home, Michelle had to use oxygen as needed for a month. She recalls being exhausted and feeling out of breath just from climbing the stairs. She didn’t start to feel normal again for about 6 months.
In July of 2023, at her 1-year checkup, Michelle was cleared to stop taking blood thinners. Transitioning off the medication was nerve-wracking. But, she says, she’s starting to feel at peace.
“I feel much calmer about it,” she says, crediting therapy and her doctor, who understands how traumatizing blood clots can be. “He never rushed me. He let me cry and say, ‘Here’s what I’m going through.’”
More and more blood clots
In late December 2017, Khelse de Prado started taking hormonal birth control. Two weeks later, as she was ringing in the new year, she realized she couldn’t tolerate drinking anything with carbonation.
“Everyone’s cheersing and I was, like, ‘Man, my belly is so full,’” says Khelse, who’s 33 and lives in Houston. “I just felt so bloated. I looked like I was 5 or 6 months pregnant.”
Khelse still didn’t feel well the next day, but she went back to work. At the time, she worked in pediatric endocrinology at a Texas hospital. One of the providers, whom she considered a mentor, took one look at her and said, “There’s something wrong with you, Khelse.” In addition to feeling bloated, Khelse was cold, and she had mottled skin on her arms. Her mentor insisted she go directly to the ER.
It turned out that Khelse had a 102-degree fever, and her blood pressure was elevated. After having a CT scan of her abdomen, Khelse was diagnosed with portal vein thrombosis. That meant that her portal vein, which is located in the abdomen, was blocked by a blood clot. It was likely caused by the birth control she had just started taking — which she never took again.
After a week in the hospital, Khelse was discharged. But her blood-clot journey wasn’t over. A year later, on Christmas Day, she experienced sharp pain shooting from her back forward through her chest.
“I felt like someone had literally punctured my heart,” she says.
Her heart was racing, and she knew she had to go to the ER. When she arrived, she was diagnosed with a pulmonary embolism. And she spent 2 weeks recovering in the hospital.
Khelse has since had deep vein thrombosis in both of her legs, as well as a blood clot in her left arm. She continues to take blood thinners, and she sees her hematologist every 3 months or so. She’s also a patient advocate with the World Thrombosis Day campaign, which aims to raise awareness about blood clots.
Her medical bills cost a lot of money, and her doctors’ appointments steal a great deal of her time. But there are positives, too, she says.
“It took me a long time to not allow this to leave me with crippling depression,” Khelse says. But “it has made me understand that I am so much stronger than I thought I was. It’s made me into a more resilient person as I work toward my goals and passions in life.”
What does the doctor say?

Patricia Pinto-Garcia, MD, MPH
Medical Editor
Blood clots can form anywhere in your body. But your body is also prepared to deal with small blood clots. You have built-in mechanisms that break down and filter small clots so they don’t cause any problems.
Larger blood clots — like those that form in the large veins in the legs — are a different story. The body can’t break down or filter these clots quickly or easily. And when a clot, or part of the clot, breaks off from its original location, it will travel to the heart and lungs. This can lead to a pulmonary embolism (PE), which is a life-threatening medical emergency.
Sometimes, people who develop blood clots in their legs — or deep vein thrombosis (DVT) — describe having unusual cramping, swelling, or pain in the leg. But most people with blood clots in their lower legs never develop any symptoms. They have no idea they had a clot until part of it travels into their lungs. Unlike DVT, a PE isn’t silent. People typically develop symptoms like chest pain and trouble breathing. Sometimes, the symptoms can be more subtle, especially at first, as the stories above show. One unique symptom of a PE is a deep, unsettling sense that something is wrong.If you’re at risk for developing a blood clot, it’s important to be aware of the symptoms of a PE and to get help as soon as you can if you notice any — even if they’re vague or mild.

Leave a Reply