By Marzia Khan
Reviewed by Danielle Ellis, B.Sc.
What is inflammation?
Inflammation is an immune response from the body’s immune system when there is a perceived injury or infection. When injured, inflammation causes the area to become red and swell due to a large number of white blood cells flowing into the area to fight against infection and aid in the healing process.
While inflammation can be caused by infection, they’re not the same, and it’s important to make this differentiation.
An infection includes bodily tissues being invaded by disease-causing organisms, followed by the multiplication of these organisms and the reaction of the body’s immune system to the organisms and the toxins they produce.
This means inflammation is typically associated with an infection, but there is not always an infection present during an inflammatory response.
The body’s defense mechanism
During an injury or infection, the immune system utilizes inflammatory cells and cytokines, which stimulate more inflammatory cells. This produces an inflammatory response in the body, which the cells use to trap germs or toxins to start healing the tissue that’s injured.
Signs of inflammation include pain, heat, redness, swelling, and loss of function. Loss of function may involve being unable to move an inflamed joint properly, losing the ability to smell during a cold, or having difficulty breathing if you have bronchitis (inflammation of the bronchi).
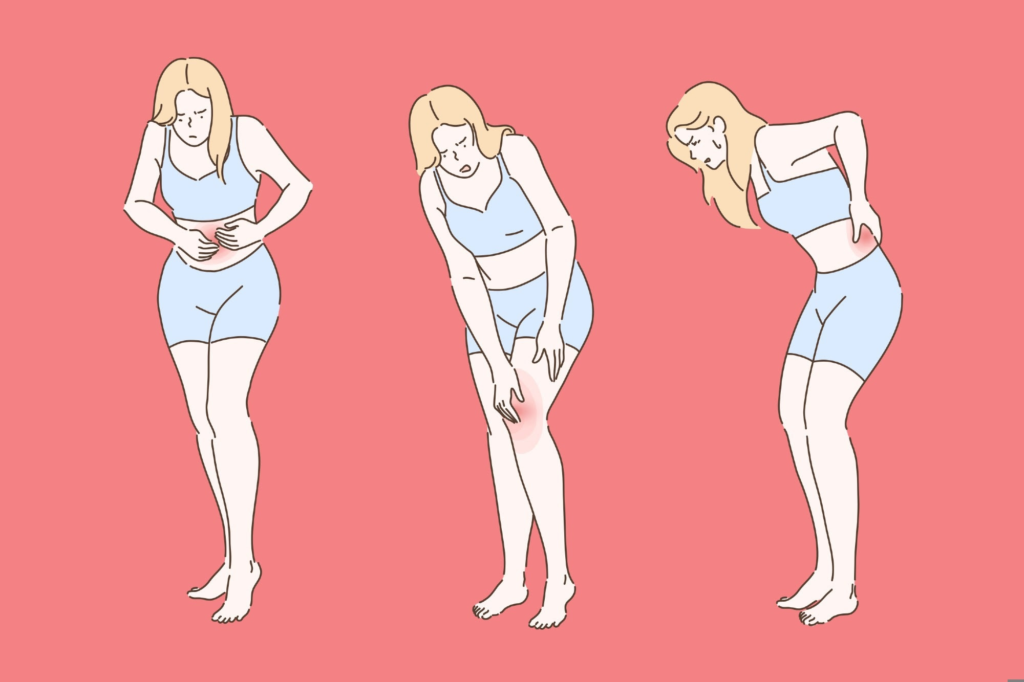
Image Credit: Vectorium/Shutterstock.com
However, an inflammatory response may not always lead to all of these five symptoms, with some types of inflammation occurring silently, without any symptoms.
The immune system may also respond to an inflammatory response by releasing inflammatory mediators from various immune cells, such as hormones like bradykinin and histamine. These hormones cause vasodilation, whereby small blood vessels in the tissue widen and allow more blood to reach the injured area – this is why inflamed areas can turn red and feel hot. Additional blood flow also enables more immune cells to migrate to the injury site to aid the healing process.
Acute inflammation: A short-term response
There are two main types of inflammation, including a short-term acute response and a longer-term chronic response.
Acute inflammation is a sudden and temporary immune response to a sudden injury or illness. This short-term response consists of inflammatory cells that travel to the injury site or an infection to start the healing process. This type of inflammation can last a few hours or a few days.
Common causes of acute inflammation include wounds such as a cut, bacterial infections such as step throat, and viral infections such as the flu, which can cause inflammation in the throat. Other types of bacterial and viral infections can also cause inflammation within the small intestine, known as enteritis.
An inflammatory response like this can be useful for the healing process, as a fever can demonstrate signs of a healthy immune system, which is very active and requires a lot of energy; this is because the rate of metabolism may be higher due to a fever, which means more antibodies and immune cells can be produced to help fight against infection.
However, it is important to be aware of immune system complications, including a rare but dangerous complication of an infection known as septicemia or blood poisoning. The signs of this complication can include chills, a very high fever, and feeling very ill.
Septicemia can occur if the bacteria that has entered the body multiplies quickly in a particular part of the body, and then a large number enters the bloodstream suddenly. A few reasons why this may occur are if the body is unable to fight the infection locally, if the immune system is weak, or if the bacteria is very aggressive.
This complication is a medical emergency and would require medical attention as soon as possible.
Chronic inflammation: A silent threat
While inflammation is a useful immune response, it doesn’t always help the body, with some diseases consisting of the immune system fighting against the body’s cells by mistake, which can cause harmful diseases.
Within chronic inflammation, the body continues to send inflammatory cells even when there is no danger. Chronic inflammation can last for months and even years, with some periods of improvement and some periods where symptoms may worsen.
Examples include rheumatoid arthritis, which is permanent inflammation of the joints, a chronic skin condition called psoriasis, and inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis.
Researchers have linked chronic inflammation to a wide range of inflammatory diseases, such as autoimmune diseases like lupus, cardiovascular diseases like heart disease, and even certain cancers.
While injuries and infections are usually the cause of acute inflammation, the root cause of most chronic inflammation cases is typically environmental factors such as aspects of daily life and toxin exposure.
Common causes of chronic inflammation include low levels of physical activity, chronic stress, having a high BMI or excess weight within the stomach area, having an imbalance of healthy and unhealthy gut bacteria, eating inflammatory foods, disrupted sleep, and exposure to toxins.
The ripple effect: Inflammation and disease
Inflammation can have a significant impact on many bodily systems, including the cardiovascular system, with cardiovascular diseases such as atherosclerosis being the leading cause of mortality worldwide.
Within atherosclerosis, inflammatory mediators hold an important role, with involvement in initial cell recruitment for the formation of plaques within blood vessels to the rupturing of vessels. Cardiac stress is manifested within the body through inflammation, demonstrating high levels of inflammatory cytokines and chemokines within affected cardiac tissues.
Coronary atherosclerosis is the most common cause of a heart attack and results in a loss of cardiac tissue. During a heart attack, inflammatory cells move to the site of the necrotic tissue to clear dead cells and debris as the cardiac cells die.
Additionally, excessive inflammatory responses to gut microbial flora can lead to polygenic inflammatory bowel disease, including Crohn’s and ulcerative colitis. Cytokines drive these two digestive diseases and can also be caused by non-infectious inflammation of the bowel.
Interestingly, increased inflammation has also been connected to depression and fatigue, with changes in the central nervous system (CNS) being seen. Inflammation can lead to increased permeability of the blood-brain barrier, which enables easier entry of inflammatory molecules or immune cells into the CNS. Inflammatory signaling within the CNS can result in structural and functional changes for those with depression and fatigue.
Inflammation also has a significant influence on chronic diseases, as previously mentioned, driving autoimmune diseases such as rheumatoid arthritis. There is also increasing evidence demonstrating inflammation as a key factor in the onset and progression of diabetes. Systematic inflammation associated with rheumatoid arthritis may also contribute to the risk of developing diabetes in the future, with markers of active inflammation such as CRP being associated with an increased risk of diabetes in those with rheumatoid arthritis.
Reducing inflammation: Lifestyle and medical approaches
Reducing inflammation is key to reducing the risk of inflammation-associated diseases.
This can include having an anti-inflammatory diet, with many foods having the ability to fight inflammation in the body, such as fatty fish such as salmon, fresh fruits, and leafy greens. This can reduce and prevent inflammation in the body, with some dieticians recommending the Mediterranean Diet or the DASH diet to reduce sodium intake and increase potassium.
Regular exercise, including 150 minutes of moderate-intensity exercise like walking per week, can lower the risk for chronic inflammation and reduce chronic stress and stress-triggered hormones. Stress management techniques include yoga, deep breathing, mindfulness, and other forms of relaxation that calm the nervous system.
Additionally, over-the-counter anti-inflammatory medications may include supplements such as zinc and omega-3, which may reduce inflammation and increase repair in the body. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also over-the-counter and can be used to reduce inflammation, along with ibuprofen, aspirin, or naproxen.
A healthcare provider may also give you a corticosteroid injection to decrease inflammation at specific joints or muscles. Healthcare providers can also prescribe prednisone to treat inflammatory conditions such as arthritis, lupus, and vasculitis.
Alleviating chronic inflammation every day through maintaining a healthy weight, exercise, a healthy diet, and low stress levels is significant for preventing inflammation-related disorders and diseases.
References
Oronsky B, Caroen S, Reid T. What Exactly Is Inflammation (and What Is It Not?). International Journal of Molecular Sciences. 2022;23(23):14905. doi:https://doi.org/10.3390/ijms232314905
Cleveland Clinic. Inflammation: What is it, causes, symptoms & treatment. Published July 28, 2021. https://my.clevelandclinic.org/health/symptoms/21660-inflammation
Harvard Health. What is inflammation, and why is it dangerous? Published March 1, 2020. https://www.health.harvard.edu/staying-healthy/what-is-inflammation-and-why-is-it-dangerous
Signore A. About inflammation and infection. EJNMMI Research. 2013;3(1):8. doi:https://doi.org/10.1186/2191-219x-3-8
Institute for Quality and Efficiency in Health Care. What is an inflammation? National Library of Medicine. Published February 22, 2018. https://www.ncbi.nlm.nih.gov/books/NBK279298/
Hannoodee S, Nasuruddin DN. Acute Inflammatory Response. PubMed. Published November 21, 2021. https://www.ncbi.nlm.nih.gov/books/NBK556083/
Lee CH, Giuliani F. The Role of Inflammation in Depression and Fatigue. Frontiers in Immunology. 2019;10(1696). doi:https://doi.org/10.3389/fimmu.2019.01696
Tian Z, Mclaughlin J, Verma A, Chinoy H, Heald AH. The relationship between rheumatoid arthritis and diabetes mellitus: a systematic review and meta-analysis. Cardiovascular Endocrinology & Metabolism. 2021;10(2):125-131. doi:https://doi.org/10.1097/xce.0000000000000244
Harvard Health. An action plan to fight unhealthy inflammation. Published May 5, 2022. https://www.health.harvard.edu/blog/an-action-plan-to-fight-unhealthy-inflammation-202205052739

Leave a Reply