by Susan Barber Lindquist, Mayo Clinic
Credit: Mayo Clinic
Frontotemporal dementia (FTD) is a group of neurologic disorders associated with changes in personality, behavior, language or movement. Some FTD forms are inherited, and some are not. Typically, people develop FTD symptoms before age 60.
While there is no cure for this progressive decline, FTD research has made significant strides in the past two decades, says Dr. Bradley Boeve (boh-VAY), a Mayo Clinic neurologist.
“There are few other neurodegenerative disorders where we have learned so much over a relatively short period of time,” says Dr. Boeve, a co-principal investigator of the ALLFTD Study, an international consortium to target FTD.
“We understand the biology of the disease that much better. The optimism for therapeutics is so much greater than even two or three years ago. There’s definitely hope.”
What are the types of FTD disorders?
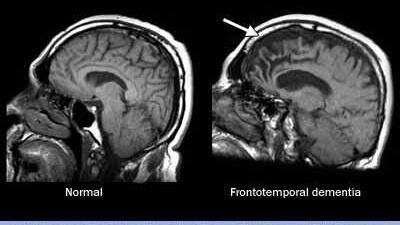
As the name suggests, FTD affects the frontal lobe and/or temporal lobes of the brain. Signs and symptoms vary, depending on which part of the brain is atrophying, or shrinking. Genetic mutations and dysfunctional proteins in the brain have been linked to FTD.
Credit: Mayo Clinic News Network
Several disorders fall under the umbrella term of frontotemporal degeneration.
Frontotemporal dementia (also known as behavioral variant frontotemporal dementia): Brain changes, primarily in the frontal lobe, cause the personality and behavior changes of frontotemporal dementia. Common signs are:
Increasingly inappropriate social behavior, Loss of empathy and other people skills, such as having sensitivity to another’s feelings
Lack of judgment
Loss of inhibition
Lack of interest (apathy), which can be mistaken for depression
Repetitive compulsive behavior, such as tapping, clapping or smacking lips
Decline in personal hygiene Changes in eating habits, usually overeating or preferring sweets and carbohydrates
“Personality (and) behavior changes tend to occur early. Disinhibited behavior—doing things that are a bit off-color or out of character for that individual,” Dr. Boeve explains. “Loss of empathy, for example, if someone were to be at a funeral, not showing the usual types of sorrow for such a somber setting.”
Primary progressive aphasia: People lose the ability to speak and write, and/or understand written or spoken language. Primary progressive aphasia also has subtypes.
“Some people have difficulties expressing language,” Dr. Boeve explains. “They comprehend reasonably well, but getting the lips and the tongue to manipulate so that words come out with fluency is more of a challenge. As opposed to another variant, coming up with the names of people or objects is the primary difficulty. (For) others, it’s a bit of a mix—comprehending, also expressing as well as naming items.”
The prevalence of behavioral variant frontotemporal dementia and primary progressive aphasia subtypes of FTD worldwide is uncertain. Estimates are between 15 to 22 per 100,000 people who are 45 to 64 years old have FTD. In the U.S., behavioral variant frontotemporal dementia and primary progressive aphasia are estimated to affect 50,000-60,000 people.
Other disorders also are grouped under the FTD umbrella:
Amyotrophic lateral sclerosis, also called Lou Gehrig’s disease, causes lack of muscle control. Muscle twitching and limb weakness or slurred speech often are the first signs.
Corticobasal syndrome results in poor coordination and stiffness in the arms or legs (often worse on one side of the body than the other), difficulty thinking, and trouble with speech and language.
Progressive supranuclear palsy causes problems with walking, balance, eye movements and swallowing.
If FTD disorders have so many similarities, how are they diagnosed?
Determining a diagnosis can be challenging. Patients with behavioral variant frontotemporal dementia sometimes are misdiagnosed with a psychiatric or stress-related illness, such as atypical depression, late-onset bipolar disorder or schizophrenia, or even midlife crisis, Dr. Boeve says.
With assistance from tests to help rule out other disorders, a doctor diagnoses a patient based on symptoms. For example, if patients are having more behavior and personality changes—with or without any language or motor problems—if they have trouble with problem-solving and judgment, but memory is relatively preserved, that’s more typical of behavioral variant frontotemporal dementia, Dr. Boeve says.
Brain imaging tests are important. An MRI scan may show shrinking of the frontal or temporal lobes of the brain. A PET scan may show metabolic changes in these same regions of the brain.
Genetic testing also is helpful. For example, the same mutated gene may cause a brother to have frontotemporal dementia and a sister to have ALS, Dr. Boeve says.
“Roughly 20% to 40% of individuals with FTD have a genetic cause or contributor, and that is more common than in Alzheimer’s disease, Lewy body disease and other neurologic disorders,” says Dr. Boeve, The Little Family Foundation Professor of Lewy Body Dementia.
Primary progressive aphasia typically can be diagnosed with language-based testing and brain imaging studies. Corticobasal syndrome and progressive supranuclear palsy can be diagnosed with a neurologic examination and brain imaging studies.
For ALS, other tests such as an electromyogram, or EMG, in addition to a patient’s symptoms and scans, may help determine a diagnosis.
On average, it takes more than three years to get an accurate diagnosis, according to the Association for Frontotemporal Degeneration (AFTD). “We often call this the diagnostic odyssey of FTD,” says Dr. Boeve, a member of the AFTD Medical Advisory Council.
What treatments are available?
No treatments are available to stop or slow FTD, but clinical trials are ongoing. Today, treatment focuses on managing symptoms.
For behavioral variant frontotemporal dementia, for example, antidepressant and antipsychotic medications may help reduce behavior problems, but all drugs have side effects, so they must be considered with caution. Medications used for Alzheimer’s disease may not be effective, which is another reason an accurate diagnosis is important, Dr. Boeve notes.
“The mainstay of therapy is nonmedication approaches—how to assist the patient and family to manage the disinhibition or the repetitive behavior, especially when in social settings or in public,” Dr. Boeve says. “It’s quite challenging for families, but those strategies can be helpful.”
Nonmedication strategies include:
Avoiding activities that trigger the undesirable behavior.
Maintaining a calm environment.
Providing structured routines.
Simplifying daily tasks.
Distracting or redirecting attention from problem behaviors.
For language problems, speech therapy may be helpful. For motor disorders, physical and occupational therapy, along with structured exercises, may help strength, mobility and balance.
How is frontotemporal dementia different from Alzheimer’s disease?
Alzheimer’s disease is more common among people 75 and older. However, people with early onset Alzheimer’s or frontotemporal dementia typically start exhibiting symptoms in midlife, from roughly age 30 to 60. Memory changes are less common with frontotemporal dementia than with Alzheimer’s disease.
In FTD, dysfunctional proteins in the brain, called tau or TDP-43, may be drivers of disease. In Alzheimer’s disease, amyloid and tau are the two dysfunctional proteins, and they can be measured in a patient’s spinal fluid. The form of abnormal tau that can be involved in FTD is different than in Alzheimer’s disease, which adds to the complexity of diagnosis when using biomarkers, Dr. Boeve says.
“There’s a profile of those proteins that are very helpful to strongly support underlying Alzheimer’s disease or strongly argue against underlying Alzheimer’s disease,” Dr. Boeve says. “We don’t have those types of fluid biomarkers based on blood testing or cerebrospinal fluid yet for FTD, although that’s an active area of research.”
What resources are available?
Support groups and medical associations for the various frontotemporal degeneration disorders can help patients, their families and care partners cope.
“Establishing an early and accurate diagnosis of FTD is the first key step,” Dr. Boeve says. “Then patients and their families can develop a comprehensive management program with their health care team. Engagement with other resources and national organizations committed to FTD care and research can provide additional methods to face the challenges ahead.”
Provided by Mayo Clinic

Leave a Reply