by Stony Brook University
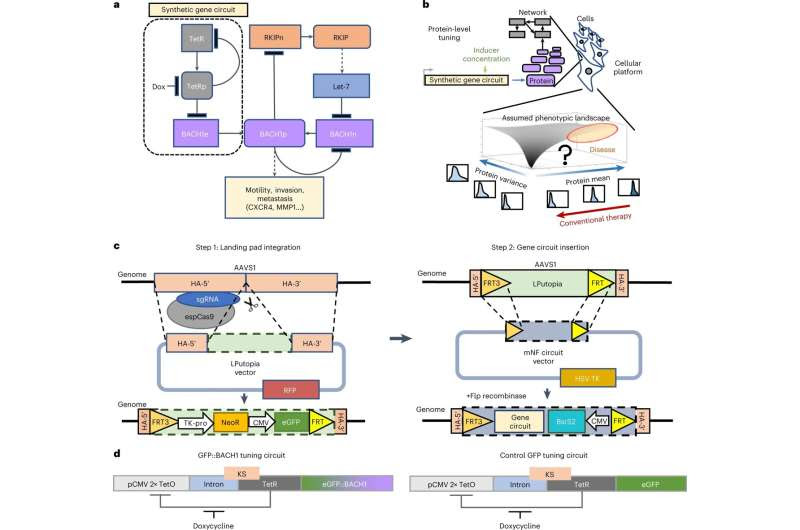
Two-step strategy for repeatable site-specific gene circuit integration. a, Network diagram of regulatory interactions and phenotypic impacts for native and ectopic BACH1. ‘BACH1e’ indicates the ectopic BACH1 gene introduced and controlled via the mNF gene circuit, whereas ‘BACH1n’ indicates the native BACH1 gene; ‘BACH1p’ indicates the BACH1 protein. The same notation applies to RKIP. b, A phenotype as a function of the mean and/or variability of one or more protein’s levels defines a phenotypic landscape. Conventional therapy assumes monotone phenotypic landscapes. However, uncovering the actual landscape requires protein-level tuning. c, Schematic diagram of the two-step strategy for repeatable AAVS1 site-specific integration of genetic payloads, such as synthetic gene circuits. Left: LP insertion into AAVS1 with CRISPR–Cas9. Right: RMCE-based LP-specific integration of the mNF gene circuit that controls the expression of the eGFP::BACH1 bifunctional fusion. Step 2 is repeatable by using different selection markers. espCas9, enhanced specificity SpCas9; NeoR, neomycin resistance gene. d, Synthetic mNF gene circuit for dox-controlled tuning of the TetR co-expressed with either the GFP reporter (mNF-GFP) protein levels or GFP::BACH1 fusion (mNF-BACH1) protein levels after site-specific integration. KS, Kozak sequence; TetO, tetracycline operator. Credit: Nature Chemical Biology (2023). DOI: 10.1038/s41589-023-01344-z
A new method than enables researchers to dial up or tone down the amount of a certain metastatic protein inhibitor (BACH1) within a cell could provide a new path in cancer research that reassesses the effectiveness of protein inhibitors to treat disease. Led by a team of Stony Brook University scientists, the research involves adjusting the levels of BACH1 using a gene circuit placed into human breast metastatic cells. Their findings are published in Nature Chemical Biology.
Biomedicine relies upon the use of protein inhibitors based on the assumption that lowering disease-promoting protein levels or activity is generally beneficial when treating cancer. But according to Gábor Balázsi, Ph.D., lead author of “Nonmonotone invasion landscape by noise-aware control of metastasis activator levels,” when it comes to oncogenes, which produce cancer-promoting proteins, manipulating them by way of an “elimination only” approach within cancer cells—the most common approach—is not necessarily the best way to develop treatments against cancer.
He and colleagues found that BACH1, which is highly expressed in many forms of metastatic cancer such as lung and breast, can be both an activator or inhibitor of cancer cell invasion in triple-negative breast cancer cells in culture.
“We developed a two-step technological pipeline that creates a kind of ‘landing pad’ in which BACH1 or other genes can be introduced safely into any human cell line, like a door that opens to the right key,” summarizes Balázsi, the Henry Laufer Professor in the Louis and Beatrice Laufer Center for Physical & Quantitative Biology, and Professor of Biomedical Engineering at Stony Brook University.
The team used various ways, including CRISPR, to genetically manipulate the cells and create the “landing pad” to complete the first step. The second step involved developing synthetic gene circuits to control the amount of protein. These circuits enabled them to employ a “dimmer switch” that controls the amount or percentage of BACH1 placed into cancer cells.
“Think of this work like a light switch, however one that works not just at ‘on’ and ‘off,’ but with a sophisticated dimmer capacity. While most research methods involving BACH1 or other cancer-promoting proteins turn the light switch on (activate) or off (inhibit), we have a fine-tuned dimmer where we can adjust the amount of the metastatic activator to intermediate percentages by way of the landing pad platform,” explains Balázsi.
What surprised the researchers in testing BACH1 in the cancer cell invasion model is that lowering the protein level did not always inhibit metastatic processes, and increasing it did not always increase cancer cell invasion.
They write, “Unexpectedly, engineered MDA-MB-231 human breast metastatic cells become more, then less and then more invasive as we tune BACH1 levels up, irrespective of the native BACH1. BACH1 expression shifts in invading cells, and expression of BACH1 transcription targets, confirm BACH1’s nonmonotone phenotype and regulatory effects. Thus, chemical inhibition of BACH1 could have unwanted effects on invasion.”
They also found that dialing up the portion of BACH1 to an intermediate level, a mid-position of the dimmer, actually inhibited the cancer invasion process, as if the light became less bright while pushing the dimmer knob up.
“Our findings provide a cautionary tale when it comes to metastasis and proteins that appear to advance the cancer process—that is, we need to take a closer look at these proteins and genes and their exact role in cancer,” says Balázsi. “It’s very possible in some cases we need to inhibit them to treat cancer, and in some cases, depending on their original levels we need to increase them, or even both, yet we need much more investigation to help determine anything conclusive.”
Their experiment showed that by applying a BACH1 degrader, it can either lower or unwantedly increase the invasiveness of breast cancer cells depending on the original level of BACH1. The authors say such results highlight the importance of characterizing the disease effects of genes by protein-level tuning.
The research involved a team of collaborators from Stony Brook and other institutions, particularly the first author, Dr. Yiming Wan. Their work was essential to the discovery highlighted in the paper.

Leave a Reply