NEWS RELEASE 16-MAY-2024
B cells drive responses of other immune cells, and can be modified to prevent Multiple Sclerosis symptoms
Abnormally active B cell metabolism causes an inflammatory immune response in individuals with MS, Penn Medicine research finds
Peer-Reviewed Publication
UNIVERSITY OF PENNSYLVANIA SCHOOL OF MEDICINE
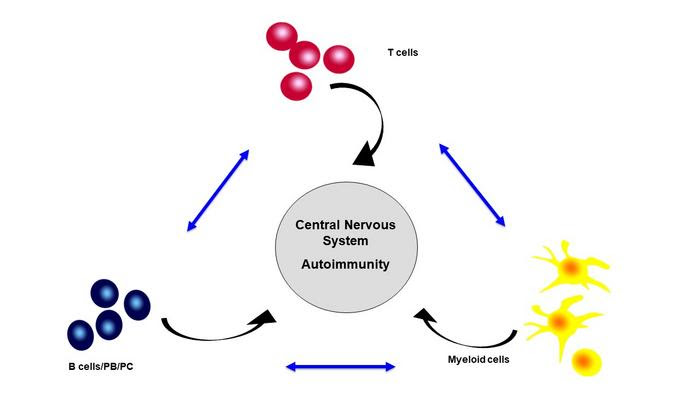
IMMUNE CELL INTERACTIONS DRIVING MS ATTACKS.
CREDIT: PENN MEDICINE
PHILADELPHIA – B cells can control responses of myeloid cells through the release of particular cytokines (small proteins that control the growth and activity of cells in the immune system), challenging the prevailing view that T cells are the principle orchestrators of immune responses. In individuals with Multiple Sclerosis (MS), abnormally active respiration in B cells drives pro-inflammatory responses of myeloid cells and T cells, leading them to attack the protective sheath (myelin) that covers nerve fibers, and leading to nerve damage that causes symptoms of MS.
An emerging class of drugs, called Bruton’s tyrosine kinase (BTK) inhibitors may alter this abnormal B cell respiration and stop the signaling that leads to MS flare-ups. The research, led by the Perelman School of Medicine at the University of Pennsylvania, was published today in Science Immunology.
“Experts previously thought that T cells were the main orchestrators of responses by other immune cell types, and that MS was principally caused by overly activated T cells,” said Amit Bar-Or, MD, a professor of Neurology, and director of Penn’s Center for Neuroinflammation and Neurotherapeutics. “This research highlights that it is actually how multiple cell types interact that matters, and that B cells modulating myeloid cells play a much more active role in the immune system than we thought.”
A healthy immune system is always responding to stimuli by activating or suppressing immune responses, in part through release of different cytokines which tell other cell types how to respond. Normally, every immune response generates a counter response, and this constant “push-me-pull-you” helps maintain the proper balance between immune responses. This way, an individual’s immune system can, on one hand, respond to an infection but also ensure that the response does not become overactive and cause damage to the body, as might occur in an autoimmune disease like MS.
In this study, researchers used both human samples and mouse models of MS to show that not only does the cytokine signaling between B cells and T cells go awry in MS, but also that B cells of MS patients produce an abnormal cytokine profile that drives myeloid cells to generate an inflammatory response.
They found that these actions can all be traced back to metabolic dysregulation in a process within the B cells called oxidative phosphorylation, a type of mitochondrial respiration. Researchers found that normal B cells can break down oxygen and release chemical energy signals that illicit a further response in the B cells themselves, and subsequently also in myeloid cells, telling them to produce a pro- or anti-inflammatory response. However, when this B cell metabolism is over-active, as it is in MS, the signaling results in abnormal myeloid as well as T cell responses which have been implicated in MS symptom flare-ups.
“An exciting approach for new MS treatments, then, might be to partially mute respiration in B cells, which could then stop the cascade of interactions between immune cells that drives inflammation and MS activity,” said Bar-Or.
The authors further showed that an emerging class of drugs, called BTK inhibitors, does just that. These agents slow overactive B cell respiration and “calm down” B cells of MS patients, so that they don’t release the same abnormal cytokine profile that drives abnormal pro-inflammatory myeloid cell and T cell responses.
Existing MS therapies, like anti-CD20 treatments, deplete B cells. However, since B cells are eliminated, the individual’s immune system may be compromised, struggling to mount certain immune responses – for example antibody responses to infections or vaccinations. In contrast, BTK inhibitors do not deplete B cells, but correct the metabolic abnormality, making the B cells less prone to drive pro-inflammatory responses of other cells.
This research was funded primarily by the Melissa and Paul Anderson Gift Fund and the National Institutes of Health Autoimmunity Center of Excellence (ACE) with partial support also from the Children’s Hospital of Philadelphia (CHOP) Center for Mitochondrial and Epigenomic Medicine grant, a grant from the National Natural and Science Foundation of China (U23A20428, 32370962, 2271845) and a sponsored research agreement between The University of Pennsylvania and Biogen.
For more information about Multiple Sclerosis research and treatment at Penn’s Penn Multiple Sclerosis and Related Disorders Center, visit: https://www.pennmedicine.org/for-patients-and-visitors/find-a-program-or-service/neurology/multiple-sclerosis.
For information on MS clinical trials at Penn Medicine, visit: https://clinicalresearch.pennmedicine.org/us/en/
Penn Medicine is one of the world’s leading academic medical centers, dedicated to the related missions of medical education, biomedical research, excellence in patient care, and community service. The organization consists of the University of Pennsylvania Health System and Penn’s Raymond and Ruth Perelman School of Medicine, founded in 1765 as the nation’s first medical school.
The Perelman School of Medicine is consistently among the nation’s top recipients of funding from the National Institutes of Health, with $550 million awarded in the 2022 fiscal year. Home to a proud history of “firsts” in medicine, Penn Medicine teams have pioneered discoveries and innovations that have shaped modern medicine, including recent breakthroughs such as CAR T cell therapy for cancer and the mRNA technology used in COVID-19 vaccines.
The University of Pennsylvania Health System’s patient care facilities stretch from the Susquehanna River in Pennsylvania to the New Jersey shore. These include the Hospital of the University of Pennsylvania, Penn Presbyterian Medical Center, Chester County Hospital, Lancaster General Health, Penn Medicine Princeton Health, and Pennsylvania Hospital—the nation’s first hospital, founded in 1751. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Penn Medicine is an $11.1 billion enterprise powered by more than 49,000 talented faculty and staff.
JOURNAL
Science Immunology
DOI
10.1126/sciimmunol.adk0865
METHOD OF RESEARCH
Experimental study
SUBJECT OF RESEARCH
Animals
ARTICLE TITLE
Oxidative phosphorylation regulates B cell effector cytokines and promotes inflammation in multiple sclerosis
ARTICLE PUBLICATION DATE
3-May-2024

Leave a Reply