by Molly Chiu, Baylor College of Medicine
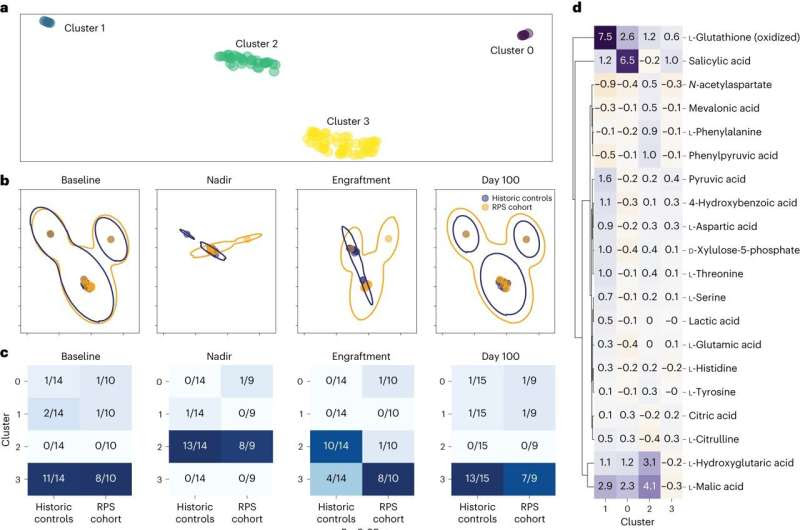
Plasma metabolites in historic controls versus recipients of RPS. a, UMAP ordination of median-centered plasma metabolite levels revealed four distinct clusters of metabolites. b, UMAP ordination stratified according to clinical group (historic controls in blue or recipients of RPS in orange), with the largest divergence in overlap at engraftment. c, Contingency tables of plasma metabolite groups stratified according to clinical group (historical controls or recipients of RPS) at four time points with baseline to the far left, followed by nadir, then by engraftment and then by day 100 to the far right. Chi-squared contingency testing P values are reported, with only significant differences between the RPS and historical control cohorts at engraftment. d, Regression revealed a subset of metabolites driving each cluster, with cluster 3 (dominant at baseline) notable for metabolite levels close to the median. Credit: Nature Medicine (2023). DOI: 10.1038/s41591-023-02587-y
Researchers at Baylor College of Medicine and the University of Michigan conducted a phase I pilot study to assess the feasibility of using potato starch as a dietary intervention to modify the gut microbiome in bone marrow transplant patients.
The study, which appears in the journal Nature Medicine, is the first part of a two-phase ongoing clinical trial evaluating the effect of modifying the microbiome on the incidence of graft-versus-host disease (GVHD), a major complication that develops in up to half the patients who receive a bone marrow transplant and can lead to injury and death.
“The gut microbiome is a community of microbes we all carry inside the body, and its composition and products affect our health,” said senior and co-corresponding author Dr. Pavan Reddy, currently professor and director of the Dan L Duncan Comprehensive Cancer Center at Baylor and previously at the University of Michigan. “Early research from our lab and others showed that a normal gut microbiome and its products change after a bone marrow transplant and that this change contributes to GVHD aggravation. Can we alter the progression of GVHD by modifying the microbiome?”
Previous pre-clinical data from the Reddy lab demonstrated that butyrate, a compound produced by healthy intestinal bacteria when they digest resistant potato starch, a form of starch that people cannot digest, was significantly decreased in the gut of mice experiencing GVHD. Restoring butyrate levels by increasing intestinal butyrate-producing bacteria reduced experimental acute GVHD severity and mortality.
“Having more butyrate in the gut is helpful for healing the intestine, and therefore beneficial for alleviating GVHD,” Reddy said. “Previous studies have also shown that in healthy people, potato starch also promotes an increase in butyrate-producing bacteria and intestinal levels of butyrate.”
These findings led the researchers to investigate whether increasing intestinal butyrate-producing bacteria and intestinal butyrate levels in bone marrow transplant patients would reduce or prevent the progression of GVHD.
“We began by assessing in the current study whether it was safe and practical for 10 patients undergoing a bone marrow transplant at the University of Michigan to take a food supplement made from resistant potato starch for more than 100 days and whether this would change the products of the gut bacteria that live in the stomach and intestine in a way that could possibly prevent GVHD after transplant,” said first and co-corresponding author Dr. Mary Riwes, clinical assistant professor in medical oncology, internal medicine and hematology at the University of Michigan’s Rogel Cancer Center.
The goal was that 60% or more of the patients would take 70% or more of the potato starch doses. “Our findings surpassed our expectations,” Reddy said. “We found that more than 80% of the patients took 84% of the doses with no negative side effects, suggesting that it is safe and feasible for most patients to regularly take the food supplement. We also found that butyrate levels in the stools were significantly higher in the participants that took potato starch than in those that did not, as we had seen both in mice and healthy adults.”
“In the next part of the study, currently open at the University of Michigan and soon to open at a second site at Baylor College of Medicine, we will determine whether taking potato starch will indeed result in less GVHD after transplant,” Riwes said.
“It’s exciting that this is the first demonstration that a simple, safe dietary intervention has an effect on the gut microbiome and metabolites in these patients,” Reddy said. “Of the 10 patients in this study, only one developed GVHD, while typically about half of bone marrow transplant patients develop the condition. We have enrolled more patients in our ongoing phase 2 clinical trial to evaluate the value of potato starch in reducing the incidence of GVHD in transplant patients.”
“We could potentially be able to use a food substance in patients undergoing a bone marrow transplant, as a simple-to-administer, low-cost and relatively safe approach to prevent GVHD, which is a major limitation to the life-saving capability of a bone-marrow transplant,” Riwes said.
More information: Mary M. Riwes et al, Feasibility of a dietary intervention to modify gut microbial metabolism in patients with hematopoietic stem cell transplantation, Nature Medicine (2023). DOI: 10.1038/s41591-023-02587-y
Journal information: Nature Medicine
Provided by Baylor College of Medicine

Leave a Reply