by Case Western Reserve University
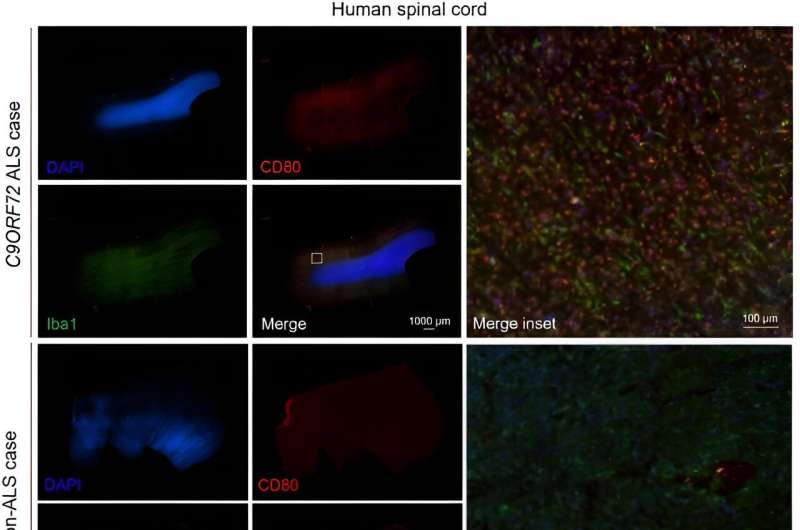
Representative human spinal cord tissue imaged at 4X objective for DAPI (blue), CD80 (red), and Iba1 (green) from an C9ORF72 ALS case and a non-ALS control. Scale bars represent 1000 µm or 100 µm as indicated. Credit: Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adg7895
Researchers at Case Western Reserve University School of Medicine have discovered why a gene, when mutated, is a common cause of two debilitating brain diseases: Amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD).
The study found that the protein generated by this mutant gene, C9ORF72, influences the immune system by regulating the production of Interleukin 17A (IL-17A), a potent inflammatory molecule.
ALS is a neurodegenerative disease that results in progressive paralysis due to the loss of neurons in the central nervous system. ALS patients often have pre-existing autoimmune disease and inflammation of the brain that worsens as muscle function declines.
Aaron Burberry, an assistant professor of pathology at the School of Medicine and the study’s principal investigator, discovered in mouse models with the C9ORF72 mutation—which affects roughly 10% of ALS patients—brain inflammation decreased and mobility improved when the IL-17A gene was blocked.
Burberry and his research team also discovered that another molecule found in the gut (CD80) contributes to inflammation in response to elevations of IL-17A in the brain. Their research was recently published in the journal Science Translational Medicine.
“Our research indicates that IL-17A blockade may be quickly repurposed to treat ALS patients to slow down the progression of their disease or possibly stop ALS from ever occurring,” Burberry said.
Treatments that block IL-17A have already been approved by the U.S. Food and Drug Administration to treat autoimmune diseases, such as psoriasis and rheumatoid arthritis. These comparable therapies may help ALS patients stop or perhaps reverse the disease’s progression.
“For people living with a neurodegenerative disease,” Burberry said, “our work offers hope for a future where quality-of-life and cognition can be maintained long after their diagnosis.”
Burberry will next investigate the mechanisms by which C9ORF72 inhibits IL-17A in lymphoid cells and identify the elements of the gut microbiome that are causing inflammation in the brain.
More information: Francesco Limone et al, Myeloid and lymphoid expression of C9orf72 regulates IL-17A signaling in mice, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adg7895
Provided by Case Western Reserve University

Leave a Reply