by Boston Medical Center
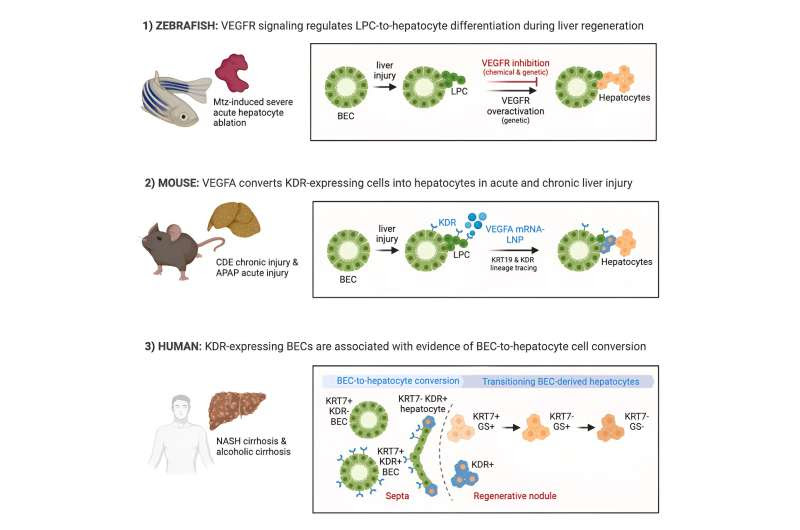
Graphical Abstract. Credit: Cell Stem Cell (2023). DOI: 10.1017/j.stem.2023.10.008
Mortality related to end stage liver disease is ranked as the 12th most common cause of death in the U.S. Liver transplantation remains the only treatment for end stage liver disease, but there is a critical shortage of organ donors, necessitating a dire need for new forms of treatment.
New research from Boston Medical Center and Boston University Chobanian & Avedisian School of Medicine’s Center for Regenerative Medicine (CReM) found evidence that a novel stem cell treatment using mRNA technology encapsulated into nanoparticles (LNP) that were successfully used to produce the COVID-19 vaccines, may boost the natural repair mechanism of the liver to regress the diseased tissue caused by either an acute or chronic liver injury.
Published in Cell Stem Cell, researchers identified a specific receptor present in the stem cells that can be recognized and activated by the ligand-protein called vascular endothelial growth factor A (VEGFA).
“This potential treatment has important clinical implications for people suffering from chronic liver disease, allowing the liver to heal itself and potentially avoiding the need for many liver transplants,” said corresponding author Valerie Gouon-Evans, Ph.D., PharmD, Director of the Boston University Liver Biologist Program, Associate Professor at Boston University Chobanian & Avedisian School of Medicine, and CReM faculty. “It’s our hope that these findings, with further study, will be translated to clinical patient care to alleviate chronic liver disease and the need for transplants as a result of acute or chronic injury.”
The liver is known for its remarkable regenerative ability through proliferation of hepatocytes. But during chronic injury or severe hepatocyte death, proliferation of hepatocytes is exhausted. To overcome this hurdle, researchers studied VEGFA as a therapeutic means to accelerate biliary epithelial cell (BEC)-to-hepatocyte conversion.
Researchers used mice and zebrafish liver disease models. In the zebrafish studies, the liver disease was created by inducing hepatocyte death with genetic and chemical intervention. The experimental group of fish was then exposed to overexpression of VEGFA, while the control group was not. Researchers observed a significant increase of newly generated hepatocytes from the BEC-derived stem cells in the presence of VEGFA.
In the mouse study, the acute disease was induced with an overdose of the drug acetaminophen, and the chronic disease was promoted with a diet. The experimental groups were treated with 2 injections of VEGFA mRNA-LNP, while the control groups were injected with neutral mRNA-LNP. Researchers demonstrated that delivery of VEGFA mRNA-LNP in both acutely or chronically injured livers induced robust BEC-to-hepatocyte conversion with a five-fold increase compared to control-treated mice and, importantly, full reversion of steatosis and fibrosis in the chronic model.
This treatment activates the stem cells of the liver, a subset of the biliary epithelial cells (BEC) lining up the liver biliary tree so that they proliferate and generate new healthy hepatocytes, the functional cells of the liver.
Nearly 30% of severe cases of acetaminophen overdose require liver transplantation because the gold standard-of-care NAC currently used in the clinic to neutralize acetaminophen toxic metabolite has a very narrow time frame of efficiency. The data suggest VEGFA mRNA-LNP as an alternative treatment for severe acetaminophen intoxication that would prevent liver failure and, thus, the need for transplantation for the many overdosed patients who come too late to the ER.
This study has critical clinical implications establishing potential novel treatments for liver diseases by exploiting and optimizing the naturally occurring BEC-mediated repair mechanism of the liver to a clinically relevant extent by delivery of VEGFA into the liver using the clinically safe mRNA-LNPs.
More information: Valerie Gouon-Evans et al, VEGFA mRNA-LNP promotes biliary epithelial cell-to-hepatocyte conversion in acute and chronic liver diseases and reverses steatosis and fibrosis, Cell Stem Cell (2023). DOI: 10.1017/j.stem.2023.10.008. www.cell.com/cell-stem-cell/fu … 1934-5909(23)00392-2
Journal information: Cell Stem Cell
Provided by Boston Medical Center

Leave a Reply