by University of Melbourne
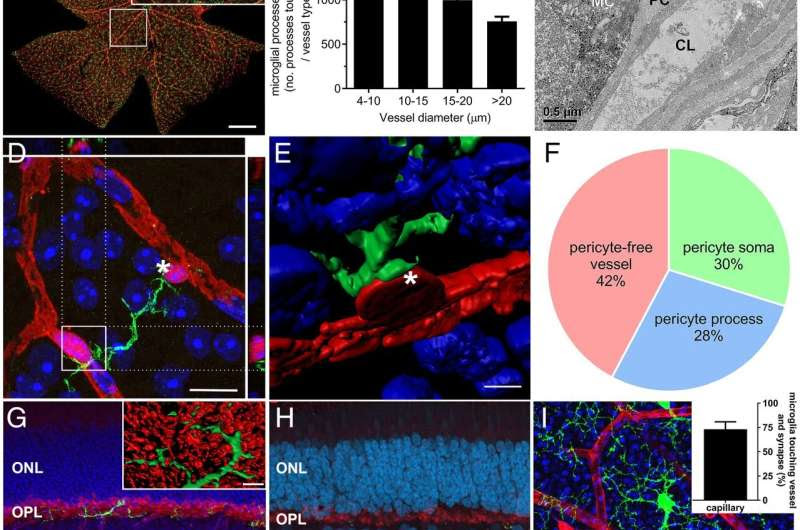
Retinal microglia associate with vasculature and neuronal synapses. (A) Whole-mounted mouse retina (Cx3cr1GFP/+) was labeled with anti-EGFP (microglia, green), and G. simplicifolia IB4 (blood vessels, red). The highlighted region shows microglial association with vessels within the superficial vascular plexus (Inset). (Scale bars, 500 µm; 50 µm, Inset.) (B) The association of microglial processes with vessels of different diameters within the superficial plexus was quantified relative to vessel area for each vessel size and show microglia preferentially associate with capillaries, *P < 0.05, ***P < 0.001. (C) The ultrastructure of microglia–vessel contact within the Cx3cr1GFP/+ retina shows microglial processes (immunolabeled against EGFP, black dots) adjoin pericytes, which contact the endothelial cells lining the capillary lumen. (Scale bar, 0.5 µm.) (D) A whole-mounted retina from the NG2-DsRed pericyte reporter mouse (pericyte somata, processes, red) stained with Iba-1 (microglia, green) and DAPI (nuclei, blue) shows a microglial process making contact with pericyte somata. The boxed region is shown in orthogonal projections (above and right). (Scale bar, 10 µm.) (E) A high-resolution–rendered image of microglial–pericyte contact taken from asterisk in D. (Scale bar, 5 µm.) (F) Microglial–pericyte interaction was further probed in rat retina and the extent of contact with pericyte somata, processes (NG2−) and capillary areas lacking pericyte contact (NG2−/IB4+) quantified. (G) A vertical section from a Cx3cr1GFP/+ retina labeled for blood vessels (IB4, magenta), microglia (EGFP, green), neuronal synapses (VGLUT1, red), and cell nuclei (DAPI, blue), showing microglia contact retinal vessels (asterisk) and neuronal synapses (arrowheads). The boxed region was imaged at higher resolution and rendered to highlight microglial–synapse interaction (Inset). (Scale bars, 50 µm; 5 µm, Inset.) (H) Neuronal–microglial–vascular contact is also observed in human retina (microglia, Iba-1, green; vessels, vitronectin, magenta, asterisk; neuronal synapses, VGLUT1, red, arrowheads; cell nuclei, DAPI, blue). (Scale bar, 50 µm.) (I) When neuronal–microglial contact was quantified in the Cx3cr1+/GFP mouse at the level of the inner retina (vessels, IB4, red; microglia, EGFP, green; neuronal synapses VGLUT1, blue), the majority of microglia contact both neuronal synapses and vessels. (Scale bar, 20 µm.) Data presented as mean ± SEM, n = 5 (B and F), n = 3 (I, Inset). GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; MC, microglia; PC, pericyte; EC, endothelial cell; CL, capillary lumen; ONL, outer nuclear layer; OPL, outer plexiform layer. Credit: DOI: 10.1073/pnas.2112561118
New research could form the basis for developing life-changing therapies that limit the impact of diabetic eye disease—a condition that could potentially affect some 1.7 million Australians, suffering from type 1 and type 2 diabetes.
Published in PNAS, University of Melbourne research uncovers how retinal immune cells change during diabetes, which may lead to new treatments that can be used from an early stage of disease, well before any loss of vision.
“Until recently, immune cells of the nervous system were thought to sit quietly, only responding when injury or disease occurred. Our finding expands our knowledge of what these cells do and shows a highly unusual mechanism by which blood vessels are regulated. This is the first time, immune cells have been implicated in controlling blood vessel and blood flow,” co-author Professor Erica Fletcher said.
Almost everyone with type 1 diabetes, and more than 60 percent of those with type 2 diabetes, will develop some form of diabetic eye disease within 20 years of diagnosis, according to Diabetes Australia. With an additional 280 people developing the disease every day, the breakthrough has important implications.
The research team found a specific type of immune cell, called microglia, contact both blood vessels and neurons in the retina and are able to change blood flow to meet the needs of neurons.
Professor Fletcher and co-author, Dr. Andrew Jobling, identified the chemical signal by which the immune cells communicate with blood vessels, and demonstrated that immune cell regulation of blood vessels is abnormal in diabetes—a disease known to affect the blood vessels in the eye. The studies used preclinical animal models and a range of imaging methods that allowed researchers to see retinal immune cells in a living eye.
“We also isolated retinal immune cells from groups of normal and diabetic animals and analyzed their genome to identify how these cells communicate with blood vessels. Finally, we used a range of pharmacological tools to examine how blood vessels change in response to activation of retinal immune cells,” Dr. Jobling said.
Professor Fletcher said the findings highlight a new way of controlling and potentially preventing retinal changes in diabetes.
“This finding also has implications for our understanding of other diseases of the retina and the brain. Although only at an early stage, these findings suggest a novel way for understanding vascular diseases of the brain with implications for our knowledge of stroke and Alzheimer’s disease,” Professor Fletcher said.
“Importantly, they were able to show that at an early stage of diabetes—before there are any visible changes at the back of the eye—blood vessels are abnormally narrow, affecting the way they supply the neurons of the retina. Retinal immune cells were implicated in this early vascular abnormality, implicating them as a novel therapeutic target for controlling early changes in the retina in diabetes.”
It is hoped the findings will help develop novel therapies for reducing the effects of vascular conditions of the retina and brain. These conditions include diabetes, Alzheimer’s disease, and vascular conditions such as stroke or retinal vascular occlusions.

Leave a Reply