by Katherine Egan Bennett, University of Texas at Arlington
Credit: Cell Reports (2023). DOI: 10.1016/j.celrep.2023.113516
A multi-institutional study co-authored by University of Texas at Arlington scientists uncovered a mechanism by which cancer cells prevent the immune system from activating and attacking the cancerous invaders.
The study, published in Cell Reports, sheds light on why immunotherapy treatments don’t work for all people or all diseases. For example, certain types of cancers—including colon, pancreatic, prostate and brain cancers—have stubbornly resisted immunotherapy. And while breast, esophageal and head and neck cancers often respond favorably, sometimes the treatments don’t work as planned. Researchers still don’t understand exactly why.
“Immunotherapy is an incredibly promising new treatment avenue for cancer, but we still have work to do determining why it doesn’t work for all people or types of cancer,” said Jon Weidanz, UTA associate vice president for research and innovation.
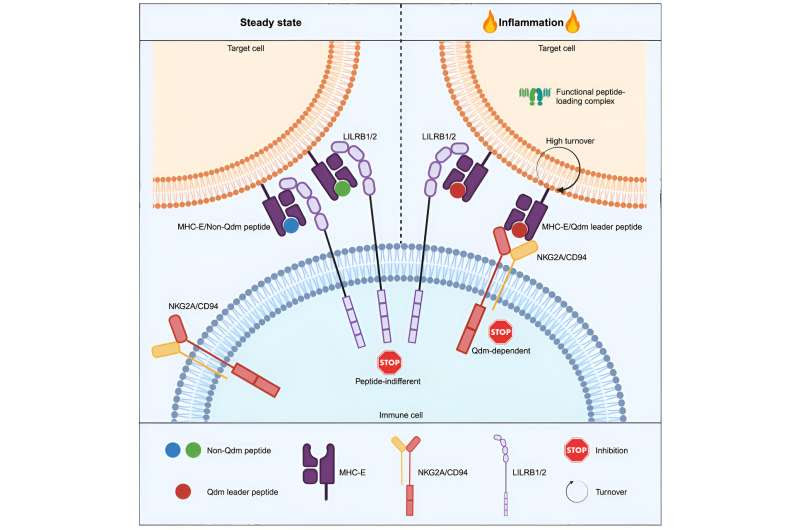
He and Soroush Ghaffari, a UTA postdoctoral fellow, were co-authors of the study, along with colleagues at Leiden University in Leiden, Netherlands, and Karolinska University in Solna, Sweden. The team determined that a key checkpoint in the immune system—called NKG2A—doesn’t engage with its specific binding molecule expressed in cancer cells until the appropriate signal is received.
Why cancer immunotherapies don’t work for everyoneJon Weidanz, UTA associate vice president for research and innovation. Credit: UT Arlington
“The team reasoned that monotherapy agents targeting the NKG2A receptor may not be effective without receiving an inflammatory trigger,” Ghaffari said. “This might explain why drugs designed to bind to the NKG2A receptor to disrupt this immune checkpoint have been only effective when used in combination with other agents that can induce the necessary inflammatory signal.”

A second major finding of the study revealed how certain cancers can inhibit the immune system from activating its macrophages, which are specialized immune cells that play a critical role in eliminating diseased or damaged cells.
“These data give us a new molecular understanding of why some immunotherapies work and some don’t,” said Weidanz, who also is a professor of kinesiology with an appointment in bioengineering and a member of the Multi-Interprofessional Center for Health Informatics.
“These results will help us identify and treat more cancers effectively with immunotherapy, helping more people live longer lives despite a cancer diagnosis.”
These findings have implications for immune system research and the development of more effective immunotherapy drugs, said Kate C. Miller, vice president of research and innovation at UTA.
“These are exciting new research results that have the potential to impact people living with cancer,” Miller said. “This is another great example of the caliber of biomedical research we’re performing both here at UTA and with our partners at other institutions.”
More information: Jim Middelburg et al, The MHC-E peptide ligands for checkpoint CD94/NKG2A are governed by inflammatory signals, whereas LILRB1/2 receptors are peptide indifferent, Cell Reports (2023). DOI: 10.1016/j.celrep.2023.113516
Journal information: Cell Reports
Provided by University of Texas at Arlington

Leave a Reply